by Charlotte Kilpatrick | Oct 24, 2024 | Technology |
The University of Connecticut (UConn) announced in October 2024 that associate Professor Thanh Nguyen’s research has received “significant” backing from The Bill and Melinda Gates Foundation. The Gates Foundation has awarded a series of grants totalling $6.6 million, following support from the National Institutes of Health (NIH) and the US Department of Agriculture (USDA). The funding will contribute to research and innovation for a microneedle array patch that can deliver multiple human vaccines at once. The Foundation initially awarded $2 million, which has increased after early success.
Microneedle array patch technology
Dr Thanh Nguyen works in the College of Engineering’s School of Mechanical, Aerospace, and Manufacturing Engineering. His microneedle method is “far less painful” than traditional syringe delivery and offers access and uptake benefits.
“What if we were able to mail people vaccines that don’t need refrigeration, and they could apply to their own skin like a bandage?”
The technology delivers highly concentrated vaccines in powder from over months, through a “nearly painless” 1-centimetre-square biodegradable patch.
“The primary argument is that getting vaccines and boosters is a pain. You have to go back two or three times to get these shots. With the microneedle platform, you put it on once, and it’s done.”
Funding increases
After the initial award of $2 million, the project made good progress and received additional funding to support the development of a scale-up manufacturing technology to produce patches on an industrial scale. In late September, the Gates Foundation awarded $4 million to take the patch “a step farther” as a pentavalent and Polio vaccine targeting diphtheria, tetanus, pertussis, HIV, Hepatitis B, and Polio. With this funding, the team can “build up productivity”. They are partnering with LTS to scale up production and are expanding the size of laboratory.
The award also marks a fundraising milestone for Dr Nguyen, who has earned more than $25 million in research awards, which he reflects “doesn’t come naturally”.
“It comes from the recognition of the high impact of the research and the lab’s success in publishing articles. It is a testament to the importance of what we are doing.”
For the latest vaccine development and technology updates, don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 24, 2024 | Global Health |
In October 2024 the International Finance Facility for Immunisation (IFFIm) priced a US$1 billion, 3-year fixed-rate bond to fund “critical vaccine research and immunisation programmes”. This is IFFIm’s largest single benchmark transaction in the primary market since its inaugural benchmark in 2006, with proceeds supporting Gavi and CEPI. The bond will mature on 29th October 2027 and carries a semi-annual coupon of 4.125% and a semi-annual re-offer yield of 4.222%.
“The success of this bond highlights the ongoing strength of IFFIm’s model, which leverages sovereign support and strong financial structuring to offer investment opportunities that make a positive impact on children’s health.”
The order book was IFFIm’s largest to date, exceeding US$4 billion. The bond drew interest from a diverse group of investors with geographic spread.
Support for vaccine programmes
IFFIm is an “important flexible tool” for organisations like Gavi; since 2006 it has provided Gavi with US$5.8 billion in financing, one sixth of its overall budget. It has been “critical” in enabling Gavi’s recent emergency responses as well as routine immunisation and health system resilience efforts. Dr Sania Nishtar, CEO of Gavi, reflected that IFFIm has been a “groundbreaking and indispensable tool”.
“Today’s bond issue provides us with vital flexibility in our mission to protect millions of children from preventable diseases and to protect our world from the threat of future pandemics.”
As Gavi nears the end of the 2021-2025 strategic period and prepares for the next phase, IFFIm states that the bond issue will play a “pivotal role” in supporting life-saving programmes.
IFFIm has also provided approximately US$272 million in past financing to CEPI in support of the research and development of new vaccines. Dr Richard Hatchett, CEO of CEPI, acknowledged the “serious threat to global health security” presented by epidemics and pandemics. He commented that these can be “mitigated through investment in vaccine R&D and manufacturing”.
“The IFFIm financing mechanism enables CEPI to access the critical funding it needs to accelerate the development of vaccines against emerging infectious disease threats, for the benefit of all.”
Offering opportunities
IFFIm Board Chair Ken Lay believes that the latest issue “highlights IFFIm’s unparalleled strengths”; it is “backed by sovereign donors, driven by a vital global mission, and structured to maximise impact”.
“IFFIm’s bonds continue to offer investors compelling opportunities to earn competitive returns with good secondary market liquidity and assured use of proceeds.”
Jorge Familiar, Vice President and Treasurer, World Bank commented that capital markets are a “powerful tool for connecting private investment with global public goods”.
“As IFFIm’s Treasury Manager, the World Bank is pleased to support IFFIm in accessing capital markets to provide a long-term and flexible funding source to Gavi to accelerate access to vaccines and vaccine development.”
Head of SSA and EMEA IG Syndicate, BofA Securities Adrien de Naurois congratulated the IFFIm team on a successful return to the USD market.
“Today’s transaction, the first USD benchmark in two years, is a clear demonstration of IFFIm’s loyal and diverse investor base, attracted by the importance of its mission to deliver immunisation programmes to those most vulnerable via the ongoing work of Gavi.”
For the latest vaccine news, don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 23, 2024 | Global Health |
A study in The Lancet Global Health sought to provide counterfactual scenarios to evaluate the short-term effects of different vaccination strategies on mpox cases and deaths in the Democratic Republic of the Congo (DRC). The researchers used a dynamic transmission model to simulate mpox transmission, stratified by age and province; this was used to assess potential vaccination strategies and their effects on deaths and cases in an epidemic year. The results indicate that vaccinating children aged 15 years or younger, or younger than 5 years, in endemic regions, would be the “most efficient use of vaccines” when resources are limited.
Mpox in DRC
Mpox was first identified in the Democratic Republic of the Congo (DRC) in 1970; it is a zoonotic infectious disease caused by the monkeypox virus (MPXV), which is endemic in “numerous regions” of west and central Africa. MPXV has two clades:
- Clade I is endemic in central Africa with an estimated case fatality rate of up to 10% and mainly affecting children. It is divided into two subclades, Ia and Ib.
- Clade II was historically found in west Africa, with an estimated case fatality rate of up to 1%-3%. It is also divided into two subclades, IIa and IIb. Clade IIb was responsible for the global mpox epidemic in 2022.
The authors state that, until 2022, MPXV was not associated with large outbreaks; most cases were related directly to sylvatic transmission from animals to humans via hunting, wild game preparation, and consumption. Increases in human-to-human transmission were identified in 2017.
The researchers suggest that the low likelihood of transmission in the early decades after the virus’ discovery could be related to smallpox eradication programmes, which offered cross-immunity via vaccination against a related orthopoxvirus. Indeed, since the cessation of the smallpox vaccination programme in the DRC, there has been a “concurrent increase in mpox cases and outbreak frequency”. There is an ongoing, “unprecedentedly large” outbreak of clade I mpox in the DRC, with more than 14,000 reported suspected cases by the end of 2023 and a 4.6% case fatality rate. Over 70% of the deaths are in children younger than 15 years.
Genetic analyses of clade Ia MPXV genomes indicate that in this outbreak, multiple, independent zoonotic introductions into the human population have occurred from one or more reservoir species. An increasing burden of clade Ib MPXV infections have been identified in eastern DRC with evidence of “sustained” human-to-human transmission and many cases in women aged 15-29 years, but clade Ia infections continue to comprise most mpox cases in the DRC.
The study
Bavarian Nordic’s modified vaccinia Ankara vaccine (JYNNEOS) is protective against mpox. It was approved by the US FDA in 2019 but was not widely used against mpox until the 2022 outbreak, when it was “quickly mobilised to vaccinate people at high risk of infection in the USA and Europe”. Despite its high efficacy at two doses, it is “largely unavailable” outside the USA and Europe.
The authors aimed to inform policy and decision makers on the “potential benefits of, and resources needed,” for mpox vaccination campaigns in the DRC. They used an approach based on models from operations research and decision science to offer a robust analysis of policy choices “even in the context of incomplete and uncertain data”. The study uses mathematical modelling to simulate the spread of mpox in the DRC during 2023.
Without vaccination, the model predicted 14,700 cases of mpox and 700 deaths from mpox in the DRC over 365 days, consistent with reported estimates. Almost 50% of the cases and deaths came from the province of Equateur. Cases were evenly split between the three age groups: 34% in children under 5 years, 32% in children aged 5-15 years, and 34% in people older than 15 years. However, deaths were “predominantly” seen in children younger than 5 years (51%).
Vaccinating 80% of children younger than 5 years in all provinces or provinces with a history of mpox cases decreased the outbreak to 10,500 cases and 400 deaths. Vaccinating in endemic provinces increased cases to 10,700 and deaths remained the same. The numbers of vaccine doses needed for the strategies were 41.4 million (all provinces), 33.8 million (provinces with a history of mpox), and 13.2 million (endemic provinces only).
Vaccinating 80% of children younger than 15 years in all provinces or provinces with a history of mpox cases decreased the outbreak to 6,400 cases and 200 deaths. Vaccinating in endemic provinces increased cases to 6,800 and deaths remained the same. The numbers of vaccine doses required for these strategies were 81.6 million (all provinces), 67.1 million (provinces with a history of mpox), and 26.6 million (endemic provinces only).
Vaccinating 80% of all ages in all provinces or only non-endemic provinces with a history of cases decreased the case burden to 1,400 cases and 100 deaths, and 2,000 cases and 100 deaths when vaccinating in provinces endemic for mpox. The numbers of doses required for these strategies were 170.8 million (all provinces), 142.0 million (provinces with a history of mpox), and 56.8 million (endemic provinces only).
Managing resources
The paper finds that vaccinating all ages leads to the “largest impact on magnitude of cases and deaths”, but that vaccinating only children aged 15 years or younger provides “nearly the same effect with fewer vaccine doses required”. Although vaccinating only children younger than 5 years showed a “drop-off” in averted cases and deaths, it provides the most efficiency.
“This analysis shows the effectiveness of focussing an mpox vaccination campaign specifically in the provinces endemic for mpox in the DRC. This targeted strategy prevents nearly as many cases and deaths as broader approaches but uses fewer vaccine doses and thus would be less costly to implement.”
Alexandra Savinkina, fourth year PhD student in the Yale School of Public Health (YSPH) Department of Epidemiology (Microbial Diseases), commented that this study could influence vaccination policy.
“My hope is that it could help inform policy for vaccination in the country and potentially the region and move the needle forward on getting vaccines to the people who need them most in the DRC.”
Savinkina hopes that “we can learn from the global mpox outbreak that we can’t ignore disease in other places”.
“If the resources to help people exist, I think we should be using them, whether in the U.S. or in Africa.”
Dr Gregg Gonsalves, associate professor of epidemiology at YSPH, acknowledged barriers to access.
“We take it for granted that we can get a vaccination for COVID or a flu shot at our local CVS, but the infrastructure to deliver vaccines in DRC is far less robust.”
For more vaccine research updates, subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 23, 2024 | Technology |
The National Institute for Health and Care Research (NIHR) announced in October 2024 that the first Phase III randomised trial of an investigational mRNA norovirus vaccine is opening across the UK. The trial seeks to evaluate the efficacy and safety of mRNA-1403 and is sponsored by Moderna. It will be conducted across 39 sites in the country, including 27 NHS primary and secondary care sites. Investigators hope to recruit 2,500 participants between late October and early 2025.
Norovirus
Norovirus, or the “winter vomiting bug”, is a viral illness; it is the “most common cause” of acute gastroenteritis globally. Symptoms include acute onset diarrhoea and vomiting, but there is evidence to suggest that norovirus infection is associated with intestinal inflammation and malnutrition and could cause long-term morbidity. WHO estimates that 685 million cases of norovirus are seen each year, including 200 million cases in children under 5.
“The burden of norovirus is significant; norovirus causes an estimated 200,000 deaths per year, including 50,000 child deaths, primarily impacting low-income countries. Norovirus has been estimated to cost $60 billion globally as a result of healthcare costs and economic losses.”
There are no licensed norovirus vaccines in use.
The trial
Participants in the trial will be randomly assigned to two groups. One group will receive the investigational vaccine, and the other groups will receive a placebo. While anyone who is aged 18 or older and meets the inclusion criteria is eligible for the trial, researchers are seeking participants aged 60 and older. This age group is “generally more likely to be severely affected by norovirus”. Thus, a successful vaccine would be of greatest benefit to them.
The trial is part of the 10-year partnership between Moderna and the UK Health Security Agency (UKHSA) on behalf of the UK Government. It is supported by the UK Vaccine Innovation Pathway (VIP) and the NIHR, which are working together to accelerate vaccine trials in the UK. The NIHR Research Delivery Network (RDN) is working with the devolved administrations to accelerate the roll-out of “key” vaccine studies. These efforts include the NIHR’s flagship recruitment tool: Be Part of Research.
Be Part of Research is an online service that connects people to health and care research across the UK. Anyone over the age of 18 can register for an account, indicating the areas of research that they are interested in. They are then sent information about suitable studies.
Advancing healthcare
The UK Chief Investigator, Dr Patrick, is a GP in Dorset and Research Director at the NIHR’s South West Regional Research Delivery Network. Dr Moore commented that the UK is “really pleased to be able to play an important role” in finding a vaccine for this “highly contagious disease”.
“Outbreaks of norovirus have huge consequences, both on our health systems and our economy. This innovative trial is crucial in helping us advance healthcare.”
NIHR Chief Executive and Chief Scientific Advisor to the Department of Health and Social Care, Professor Lucy Chappell, hopes that the vaccine could “make a difference to lives of many – especially our most vulnerable citizens”.
“Leveraging the UK’s expertise in vaccine development, the DHSC through the NIHR and Moderna are delivering this large-scale trial at pace, so that people across the UK and the world can benefit sooner.”
Health and Social Care Secretary Wes Streeting described the trial as a “huge vote of confidence in the UK’s life sciences sector”. It could also allow a “shift” away from sickness towards prevention, which would reduce pressure on the NHS and keep people healthier in the colder months. Moderna’s Chief Development Officer Dr Melanie Ivarsson is “delighted” to bring the trial to the UK.
“By advancing our investigational mRNA norovirus vaccine into a pivotal Phase III trial, we are one step closer to potentially providing a new tool to prevent infection from this highly contagious virus, which places a significant burden on health systems globally.”
Sarah Collins, Commercial Director at UKHSA, reflected that norovirus “isn’t just a nasty tummy bug – it can have serious consequences” including “disruption” to health services and education settings.
“It’s fantastic to see the first trial of its kind get underway as a result of UKHSA’s strategic 10-year partnership with Moderna, which aims to enhance investment in scientific research and vaccine development to enable a rapid response to future pandemics and other infectious diseases.”
For the latest on vaccine research, don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 21, 2024 | Global Health |
In October 2024 WHO certified Egypt as malaria-free after a “nearly 100-year effort” by the government and people to end the disease. WHO described this as a “significant public health milestone” for the country’s more than 100 million inhabitants. Egypt is the third country to receive this certification in the WHO Eastern Mediterranean Region, following the United Arab Emirates and Morocco.
Across the globe, 44 countries and 1 territory have achieved this status by proving beyond reasonable doubt that the chain of indigenous malaria transmission by Anopheles mosquitoes has been interrupted nationwide for at least the previous three consecutive years. A country must also demonstrate its capacity to prevent the re-establishment of transmission.
Malaria becomes history
WHO states that malaria has been traced back as far as 4000 BCE in Egypt; there is genetic evidence of the disease in Tutankhamun and other ancient Egyptian mummies. More recently, efforts to reduce human-mosquito contact began in the 1920s with the prohibition of rice cultivation and agricultural crops near homes. With much of the population living along the banks of the Nile River and malaria prevalence “as high as 40%”, malaria was designated as a notifiable disease in 1930.
By 1942, malaria cases in Egypt exceeded 3 million due to population displacement caused by the Second World War, the disruption of medical supplies and services, and the invasion of Anopheles arabiensis, which is a “highly efficient mosquito vector”. Egypt responded to the outbreak by establishing 16 treatment divisions and recruiting more than 4000 health workers. The Aswan Dam, completed in 1969, brought an additional risk of malaria as standing water provides a mosquito breeding ground. Thus, Egypt worked with Sudan to launch a “rigorous” vector control and public health surveillance project.
By 2001, malaria was “firmly under control”, encouraging the Ministry of Health and Population to work on preventing the re-establishment of local malaria transmission. Egypt “rapidly” contained a small outbreak in the Aswan Governorate in 2014. The recent certification recognises continued efforts and initiatives including the free provision of malaria diagnosis and treatment to the population, regardless of legal status, and health professionals’ training to detect and screen for malaria. The country also has “strong” cross-border partnerships with neighbours like Sudan, which have been “instrumental”.
The beginning of a new phase
Dr Tedros Adhanom Ghebreyesus, WHO Director-General, congratulated Egypt on its achievement.
“Malaria is as old as Egyptian civilisation itself, but the disease that plagued pharaohs now belongs to its history and not its future. This certification of Egypt as malaria-free is truly historic, and a testament to the commitment of the people and government of Egypt to rid themselves of this ancient scourge.”
Dr Tedros hopes that this will be an “inspiration to other countries in the region”, showing “what’s possible with the right resources and the right tools”. Deputy Prime Minister of Egypt H.E. Dr Khaled Abdel Ghaffar commented that the certification is “not the end of the journey but the beginning of a new phase”.
“We must now work tirelessly and vigilantly to sustain our achievement through maintaining the highest standard for surveillance, diagnosis and treatment, integrated vector management, and sustaining our effective and rapid response to imported cases. Our continued multisectoral efforts will be critical to preserving Egypt’s malaria-free status.”
Dr Abdel Ghaffar reaffirmed that the country will “continue with determination and strong will”. WHO Regional Director for the Eastern Mediterranean Dr Hanan Balkhy emphasised that the success is “not just a victory for public health but a sign of hope for the entire world”, including other endemic countries in the region.
“This achievement is the result of sustained, robust surveillance investments in a strong, integrated health system, where community engagement and partnerships have enabled progress. Furthermore, collaboration and support to endemic countries, such as Sudan, remain a priority.”
For insights into the latest malaria vaccine development progress, join us at the Congress in Barcelona next week. Don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 21, 2024 | Therapeutic |
Research in Nature in October 2024 leverages evidence that bacteria “naturally home in on tumours and modulate antitumour immunity” to explore potential vaccine applications. The authors engineered a probiotic Escherichia coli Nissle 1917as an antitumour vaccination platform, revealing a promising immune response. In mouse models of advanced colorectal cancer and melanoma, the vaccine triggered the immune system to suppress the growth of primary and metastatic cancers. The team hopes that this research can advance personalised cancer vaccine approaches.
Bacteria as ideal vectors
The authors identified bacteria as “ideal vectors to augment and direct” antitumour immune responses thanks to their support of the activation of both innate and adaptive immunity. Furthermore, bacteria can be synthetically engineered with ease for “safe delivery” of immunomodulatory compounds. Although various tumour neoantigen vaccines have demonstrated “promising” clinical trial results, benefit is “limited to only a subset of patients”. Thus, programming bacteria with genetic directives to release high levels of specific tumour neoantigens offers a system for the precise instruction of neoantigen targeting in situ.
The study
The researchers developed an engineered bacterial system in probiotic Escherichia coli Nissle 1917 (EcN) to “enhance expression, delivery, and immune-targeting of arrays of tumour exonic mutation-derived epitopes”. These epitopes are “highly expressed” by tumour cells and predicted to bind major histocompatibility complex (MHC) class I and class II. The system engages several “key design elements” to enhance therapeutic use:
- Optimisation of synthetic neoantigen construct form with
- Removal of cryptic plasmids and deletion of Lon and OmpT proteases to increase neoantigen accumulation
- Increased susceptibility to phagocytosis for enhanced uptake by antigen-presenting cells (APCs) and presentation of MHC class II-restricted antigens
- Expression of listeriolysin O (LLO) to induce cytosolic entry for presentation of recombinant encoded neoantigens by MHC class I molecules and T helper 1 cell (T H1)-type immunity
- Improved safety for systemic administration due to reduced survival in the blood and biofilm formation
Through exome and transcriptome sequencing of subcutaneous CT26 tumours the researchers developed a repertoire of neoantigens, which were predicted from highly expressed tumour-specific mutations. They then endeavoured to create a microbial system that could “accommodate the production and delivery of diverse sets of neoantigens” to lymphoid tissue and the tumour microenvironment (TME).
“Synthetic neoantigen construct optimisation and genetic engineering achieved a microbial platform (EcNcΔlon/ΔompT/LLO+) capable of robust production across diverse sets of tumour neoantigens, which was attenuated in immune-resistance mechanisms, effectively taken up by and proficient in activating APCs, and able to drive potent activation of T cells specific for encoded recombinant antigens to support enhanced cellular immunity.”
Vaccine applications
The study revealed that antigen sets encompassing predicted MHC-II and MHC-II binding neoantigens mediated antitumour efficacy. Enhanced frequencies of neoantigen-specific CD4+ and CD8+ T cells were seen. Across distinct tumour models and genetic backgrounds, the antitumour effect of vaccination was “accompanied by broad modulation of the immune compartment within the TME”.
“The coordinated regulation of APCs, reduction of immunosuppressive myeloid, regulatory T and B cell populations, and activation of NK cells and CD4+ and CD8+ T cells together indicate the advantage of precisely engineered microbial platforms as next-generation antitumour vaccines that align several arms of immunity.”
Furthermore, the “unique ability” of microbial vaccines to “directly remodel” the TME could “promote synergy” across various forms of immunotherapy. Microbial neoantigen vectors locally increase neoantigens density, recruit and activate dendritic cells and CD4+ and CD8+ T cells, and reduce immunosuppressive populations and ligands within the TME. Therefore, in combination with adoptive T cell therapy (ACT), they could “oppose these resistance mechanisms and provide synergistic benefit”.
“Through extra programming of the microbial vectors and rational incorporation of other immunotherapeutics, this system may achieve reliable eradication of established solid tumours and metastases through precision cancer immunotherapy using living antitumour vaccines.”
Getting closer
Jongwon Im, PhD student at Columbia University, helped lead bacterial engineering aspects of the study, and commented on the “net effect”.
“The bacterial vaccine is able to control or eliminate the growth of advanced primary or metastatic tumours and extend survival in mouse models.”
These vaccines are personal, programmed to “direct the immune system” to target “distinct genetic mutations”, said Dr Nicholas Arpaia, associate professor of microbiology and immunology at Columbia University’s Vagelos College of Physicians and Surgeons.
“As we continue to integrate additional safety optimisations through further genetic programming, we are getting closer to the point of testing this therapy in patients.”
Dr Tal Danino, associate professor of biomedical engineering at Columbia’s School of Engineering, reflected that the time to treatment will “first depend on how long it takes to sequence the tumour” for each patient.
“Then we just need to make the bacterial strains, which can be quite fast. Bacteria can be simpler to manufacture than some other vaccine platforms.”
Another benefit of bacteria is the enabled delivery of a “higher concentration of drugs that can be tolerated when these compounds are delivered systemically throughout the entire body”, suggested Dr Arpaia.
“Here, we can confine delivery directly to the tumour and locally modulate how we’re stimulating the immune system.”
For the latest insights into cancer vaccine research make sure you join us at the Congress in Barcelona next week, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 18, 2024 | Global Health |
The Global Polio Eradication Initiative (GPEI) announced the “difficult decision” to extend the timelines needed to achieve polio eradication. This decision, made by the Polio Oversight Board (POB) in July 2024, was shared in October 2024 with an update to funding requirements. Although GPEI recognised the “unprecedented progress” made so far, it highlighted the danger of falling into an “unacceptable future”, demanding collaboration and support for the next stages of eradication efforts.
Progress against polio
GPEI commented that “for more than three and a half decades” it has been supporting governments and health workers to make “unprecedented progress toward the promise of a polio-free world”. Through this work, more than 20 million people are “walking who would otherwise have been paralysed by this dreadful disease”. “Billions” of children have benefitted from lifesaving immunisations, and five out of six WHO Regions are free from wild poliovirus.
Closing the gaps
With broad global success, the programme is largely now “concentrated in some of the most complicated and fragile settings in which to deliver basic healthcare”. It faces “serious”, from “persistent violence to climate emergencies”. Indeed, the transmission of polio in conflict-affected areas in Gaza, Sudan, and Yemen, provides a “stark reminder” that “where conflict debilitates health and sanitation systems, polio will inevitably appear” unless eradication of all forms of the virus can be achieved.
Extended timelines
In recognition of the continued challenges, the GPEI’s POB decided to extend the timelines needed to achieve polio eradication to the end of 2027 (wild poliovirus) and the end of 2029 (type 2 variant poliovirus). The decision, made in July 2024, was informed by “critical analysis and expert consultations”. The consequence of this extension is a need for further financial resources.
In October 2024, the POB determined that the total funding needs of the extended 2022-2029 strategic period are US$6.9 billion; this is an increase from the US$4.8 billion projected for the 2022-2026 strategic period. Donors have already committed an “incredible” US$4.5 billion, leaving US$2.4 billion “urgently needed”. The funds will enable the programme to make “tactical shifts”, allowing GPEI to:
- Reach more children with polio vaccines by working with polio-affected country leaders to strengthen programme implementation
- Deploy innovative tools like novel vaccines and surveillance methods to further strengthen outbreak response
- Improve accountability at all levels, from global leadership to field managers
- Work with routine immunisation programmes by integrating polio services where possible
- Deepen relationships by strengthening community engagement
These “shifts” are driven by partners’ expertise and a “programme-wide commitment to double down on the toughest but most critical challenges”.
GPEI warns that shortcomings in funding or executing these efforts would have “serious consequences”.
“Without dedicated eradication efforts, within a decade, many thousands of children around the world could once again be paralysed or die from polio each year. This is an unacceptable future.”
The importance of donor and polio-affected country governments supported is highlighted as central in reaching all children with lifesaving vaccines and strengthening health systems in the process.
“With strengthened support and collaboration, together we can deliver a world where all children, families, and communities are forever free from polio.”
For the latest vaccine and global health updates, don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 18, 2024 | Technology |
In October 2024 the Animal and Plant Health Agency (APHA) and The Vaccine Group (TVG) announced that Innovate UK has awarded them a Smart grant in excess of £400,000 to advance a novel viral vector platform. In a project lasting 19 months, the two organisations will use technology developed by TVG scientists in candidate vaccines for two “important diseases in cattle”: bovine respiratory syncytial virus (BRSV) and lumpy skin disease (LSD). The project will continue previous research, which identified potential vaccine candidates; it is supported by the World Reference Laboratory for Non-Vesicular Diseases at The Pirbright Institute, determining how the candidates can produce an adequate serological response in animals and protect cattle.
BRSV and LSD
Bovine respiratory syncytial virus (BRSV) is the leading viral cause of respiratory illness in young calves in the UK. It affects around 1.9 million calves each year, costing approximately £54 million. It is “prevalent worldwide” and poses a “substantial economic burden” on beef and dairy producers. In the past 10 years, lumpy skin disease (LSD) has spread “dramatically” beyond former natural enzootic geographies in Africa and the Middle East to cause “severe disease” in other regions.
Both diseases have “broad global prevalence”, and BRSV particularly affects intensively reared cattle. Currently available commercial vaccines for BRSV do not prevent shedding and are restricted from use in young calves by maternal immunity. There are no DIVA (differentiating infected from vaccinated animals) vaccines available for LSD, so use is limited to areas where serosurveillance and eradication programmes are in place.
TVG’s vaccine solutions
The Vaccine Group (TVG) hope to address these challenges. With “key opinion leaders” for the two diseases in the UK and Canada, TVG has inserted transgenes for protective antigens from each virus into two separate constructs through genetic manipulation. Both vaccine candidates have been shown to be genetically stable and have demonstrated “stable and prolonged” protein expression in tissue culture over multiple passages. The technology works by introducing a benign virus to cattle, which stimulates the expression of proteins to induce an immune response.
Chief Executive Officer at TVG, Dr Jeremy Salt, reflected that infectious diseases are a “major cause for concern” for cattle farmers around the world, leading to “significant losses – both in terms of animal health and welfare, and in financial terms”.
“Our goal in developing a viral vector platform for use in cattle effective vaccines is to overcome some of the deficiencies that affect the current commercialised vaccines. By doing so, we can better protect the farmers, their animals, and their livelihoods.”
Dr Salt also hopes to “make beef and milk production more efficient, humane, and sustainable”, whilst “helping the sector address the global challenges of antibiotic resistance and carbon emissions”.
We look forward to hearing from Dr Salt at the Congress in Barcelona in just a few weeks; get your tickets to join us there and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 17, 2024 | Technology |
Valneva and LimmaTech Biologics announced in October 2024 that they have been granted Fast Track designation by the United States FDA for Shigella4V (S4V). S4V is “the world’s most clinically advanced” tetravalent bioconjugate shigellosis vaccine candidate. In August 2024 the two organisations announced a strategic partnership and exclusive licensing agreement to develop, manufacture, and commercialise S4V. The FDA designation is granted to products in development that have the potential to treat serious conditions and fill an unmet medical need, with the goal of facilitating clinical development and expediting review.
Addressing a global health threat
An estimated 165 million cases of disease and 600,000 deaths are attributed to Shigella every year; the greatest burden is among children in low- and middle-income countries (LMICs). Shigellosis also affects international travellers from high-income countries and deployed military personnel in endemic regions.
Thomas Lingelbach, Chief Executive Officer of Valneva, stated that shigellosis is the “second leading cause of fatal diarrhoeal disease worldwide” with no approved Shigella vaccine.
“The development of Shigella vaccines has been identified as a priority by the World Health Organisation (WHO). Fast Track designation allows us to work closely with the FDA to accelerate our efforts to deliver a preventative solution against this deadly disease.”
Dr Franz-Werner Haas, Chief Executive Officer of LimmaTech, is “highly encouraged” by the designation, which “reinforces our efforts”.
“[It] underscores the significant potential of the S4V Shigella vaccine candidate to address a serious global health threat.”
The way forward
After positive Phase I/II results earlier in the year, LimmaTech will conduct a Phase II Controlled Human Infection Model study (CHIM) in the United States and a Phase II paediatric study in LMICs. These are expected to begin before the end of 2024. Valneva will assume all further development, including chemistry, manufacturing, and controls (CMC) and regulatory activities. It will also be responsible for global commercialisation if the vaccine is approved.

by Charlotte Kilpatrick | Oct 17, 2024 | Global Health |
A study in The Lancet Global Health estimates the impact that the 100 Days Mission could have had on the COVID-19 pandemic. The authors find that the implementation of non-pharmaceutical interventions (NPIs) within the 100 Days Mission could have averted around 8.33 million deaths, corresponding to a monetary saving of US$14.35 trillion. Investment in manufacturing and health systems contribute an increase to 11.01 million deaths averted. The researchers comment on the value of the 100 Days Mission but emphasise the importance of “prioritising a more equitable global vaccine distribution”.
In search of greater vaccine benefits
Although COVID-19 vaccines are estimated to have prevented almost 20 million deaths, the authors demand a better understanding of the “further health and economic benefits that could have been achieved” through shorter development times and “improved global equity in pandemic preparedness”. CEPI’s 100 Days Mission was proposed in 2021, establishing the ambition of cutting vaccine development time for new pathogens to 100 days. This about a third of the time taken to deliver the first COVID-19 vaccine.
“The availability of COVID-19 vaccines within 100 days would have substantially changed the pandemic; however, these benefits would be finite without enabling equitable access to vaccine products through system equity.”
Various efforts to encourage global vaccine distribution were “hampered” by inequities, and it is recognised that manufacturing capacity should be “expanded but also diversified” to “promote self-sufficiency and regional resilience”. Furthermore, supply chains and infrastructure must be scaled to enable the delivery of vaccines that rely on cold-chain infrastructure.
The study
The searchers hoped to quantify the potential impact of the 100 Days Mission by retrospectively estimating the effect it would have had on the COVID-19 pandemic, thus offering evidence to support decision making around future investments in research and development capabilities. They also aimed to quantify the impact of “additional investments”.
The analyses use an extended version of a previously published compartmental susceptible-exposed-infectious-recovered transmission model of COVID-19 vaccination with an explicit healthcare pathway. The vaccination pathway was expanded to include booster vaccination alongside waning efficacy, capturing the “restoration of immunity” through booster doses. The new vaccination pathway was parameterised to match platform-specific vaccine efficacy data and the duration of protection.
The authors modelled the impact of the 100 Days Mission by simulating a counterfactual scenario where the global vaccination campaign began on 20th April 2020, 100 days after the publication of the full SARS-CoV-2 genome. This scenario assumes that vaccinations in each country took the same roll-out process, but 232 days earlier. Two additional scenarios reflected “increased investment” in research and delivery infrastructure.
The Manufacturing scenario removed supply constraints, enabling the rollout of vaccination on 20th April 2020 in every country, without stockouts. The infrastructure-equity scenario enhanced both national health systems and global distribution networks so that all countries achieved 40% vaccine coverage in the first year and 40% booster coverage in the second year.
To account for the relaxing of non-pharmaceutical interventions (NPIs), the authors simulated three scenarios for NPI relaxation speeds as vaccination coverage improved. The History scenario assumed no changes, whereas the Target and Economic scenarios assumed earlier relaxing; the Target scenario lifted all restrictions over two months after reaching more than 80% adult coverage in high-income countries or more than 80% coverage in those older than 60 in other countries. The Economic scenario lifted NPIs more gradually after reaching the over-60 target, prioritising the reopening of schools.
Study findings
The results suggest that the 100 Days Mission could have averted an additional 8.33 million deaths due to COVID-19 by the end of 2021 when combined with the History NPI lifting scenario. In this scenario, an estimated 26.72 million severe cases of COVID-19 requiring hospitalisation and 1/44 billion infections would have been averted. Most of these averted deaths, hospitalisations, and infections would have occurred in low- and middle-income countries (LMICs).
The estimated VSLs (value of a statistical life) that could have been saved by the 100 Days Mission through the History scenario is US$22.61 trillion globally. As VSLs are “significantly higher” in HICs, 57% of the global value of statistical life averted occurred in HICs, even though most deaths would have been averted in LMICs. To estimate the monetary values associated with lives saved the authors multiplied the number of lives saved by the country-specific monetary VSL and by the value of a statistical life-year (VSLY).
“Increased investment in both global manufacturing and health systems infrastructure further increases the number of deaths that could be averted and the associated health-economic savings.”
In the 100 Days Mission with both manufacturing and health systems investments, an estimated 11.01 million deaths could have been averted and a value of $31.29 trillion in statistical lives saved. However, the authors describe this scenario as “unlikely”. In all scenarios involving the relaxing of NPIs thanks to earlier availability of vaccines, additional lives would have been saved.
In the Target NPI lifting scenario, an estimated 5.76 million deaths (100 Days Mission alone) to 9.20 million deaths (100 Days Mission with both manufacturing and infrastructure investments) could have been averted. In these scenarios, 12,600 and 23,900 fewer days of NPIs would have been implemented globally: 70 days and 133 days on average per country. Under the Economic scenario there were “similar trade-offs between public health and economic gains”. The public health and health economic outcomes would be greater than under the Target scenario, but still lower than the History scenarios.
Substantial benefits
“Earlier access to COVID-19 vaccines could have had substantial benefits.”
Most of the estimated averted deaths would have been concentrated in LMICs, but this demands investments in vaccine research, supported by “improvements to manufacturing and health system infrastructures”. With these investments, the authors estimate that 11 million deaths could have been prevented globally.
Although NPIs were effective at reducing transmission they incurred “significant economic and societal costs”, including consequences for education. Therefore, a major benefit of earlier access to vaccination is the reduction in school closures; in the Economic scenario, prioritising school opening could have averted 1,120 weeks of full school closures and 2,490 of partial school closures. This represents an average of 6 weeks of fully open schools and 14 weeks of partly open schools per country.
“Reopening schools and relaxing NPIs safely will crucially require scaling up both vaccine delivery infrastructure and manufacturing. Without addressing both aspects, advancements in vaccine development speed might not translate into equitable benefits globally.”
The results emphasise the importance of investments in support of the 100 Days Mission in controlling a future potential pandemic, with benefits for both health and economy.
“The 100 Days Mission is ambitious, requiring global innovation through creating vaccine libraries, clinical trial networks, accelerated immune response marker identification, rapid vaccine manufacturing, and strengthened global disease surveillance.”
CEO of CEPI, Dr Richard Hatchett, hopes that this research will encourage global commitment to the 100 Days Mission.
“This work shows in the starkest terms why the world needs to be prepared to move faster and more equitably when novel pandemic disease threats emerge. Investing in preparedness now to make the 100 Days Mission possible for future incipient pandemics will save millions upon millions of lives and protect the global economy against catastrophic losses.”
Join us at the Congress in Barcelona this month to explore how lessons from the COVID-19 pandemic can inform better global preparedness for pandemic and epidemic pressures, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 16, 2024 | Global Health |
In October 2024, parliamentarians from across the world met at the UNITE Global Summit in Berlin to sign a statement in support of the WHO Pandemic Agreement. The statement was described by WHO as a “significant commitment” to “strengthen pandemic preparedness, response, and equitable access to health”. The Summit was held in collaboration with the World Health Summit (WHS), drawing global parliamentarians, civil society leaders, and health experts to “translate discussions into actionable policy priorities”.
Building trust for a healthier world
The World Health Summit 2024 was held under the theme “building trust for a healthier world”, focussing on inspiring “innovative solutions for better health and well-being for all”. The UNITE Global Summit agenda reflected key topics highlighted during WHS, divided into four pillars:
- Human rights and equitable access to health
- Global health architecture and security
- Strengthening of healthcare systems
- Sustainable financing for health
Support for the Pandemic Agreement
The Pandemic Agreement is under negotiation by WHO Member States as an attempt to address the “gaps” exposed by the COVID-19 pandemic and the threats presented by mpox and other disease outbreaks. It also seeks to “strengthen global collaboration pandemic prevention, preparedness, and response”.
A critical moment during the summit was the signing of the Global Parliamentary Statement in Support of the Pandemic Agreement, which demonstrated the importance of parliamentarians in “ensuring global health security and safeguarding populations against future pandemics”. The statement emphasised their commitment to ensuring that “all countries, regardless of resources, have access to the tools, capacities, resources, and healthcare required” during a pandemic.
Dr Ricardo Baptista Leite, President of UNITE, commented that parliamentarians are the “voice of the people” and carry a “crucial responsibility in safeguarding public health”.
“The WHO Pandemic Agreement represents a historic opportunity to prevent pandemics and strengthen our global preparedness and response capabilities. By signing this statement, we are not only showing our support for the agreement but also pledging to ensure that its principles of equity, solidarity, and global cooperation are fully realised in every nation.”
WHO Director-General Dr Tedros Adhanom Ghebreyesus welcomed the support for the “once-in-a-generation opportunity to build a stronger, fairer, and more prepared global health system”.
“By signing this statement, parliamentarians from around the world are showing their commitment to protecting lives from future pandemics and ensuring equitable access to vaccines, treatments, diagnostics, and other health tools for every country, particularly those with fewer resources.”
Key commitments
The Global Parliamentary Statement emphasises four “key commitments”:
- Equity at the core – ensuring equitable access to pandemic-related health tools based on public health need for everyone, especially countries with fewer resources
- Global solidarity – strengthening international cooperation to build resilient health systems that can prevent and respond to pandemics
- Legislative action – advocating for the ratification and implementation of the Pandemic Agreement within national legislatures, as appropriate
- Combating misinformation – providing communities with evidence-based health information to counter the spread of harmful misinformation
Dr Baptista Leite reflected that “the challenges we face today demand a global response”.
“No single country can prevent or combat pandemics alone. The WHO Pandemic Agreement is an essential step forward in ensuring that every nation has the tools, resources, and capabilities to respond to future health threats.”
More work to be done
WHO states that the Pandemic Agreement “needs to continue to garner broad international support”. Within the latest commitment, parliamentarians are to work with WHO and other international organisations to ensure the Pandemic Agreement is implemented in a way that “benefits all countries”, particularly those with “limited resources”.
“The statement signed in Berlin is expected to act as a catalyst for global parliamentary action, fostering collaboration and solidarity among nations.”
Join us at the Congress in Barcelona this month for a keynote discussion on “strengthening global preparedness and building resilient health systems” with experts from the field, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 16, 2024 | Technology |
CEPI announced in October 2024 that it is working with experts at the National Research Council of Canada (NRC) to bioengineer a “commonly used approach” to safely make protein antigens in “as little as two weeks”. This would be between eight and twelve times faster than the current timeline of antigen production for protein-based vaccines. CEPI is contributing up to CAD $850,000 and the NRC is providing up to CAD $308,000 (in kind) to establish proof-of-technology.
Low cost and high speed
CEPI notes the importance of manufacturers being able to make “sufficient quantities” of vaccine components at low cost to enable mass production. Although mammalian cell lines are a common choice for vaccine processes, boasting ease of culture and a high production yield, they can take four to six months to develop and optimise for antigen production. This is a “major challenge” to efforts to develop vaccines quickly in response to fast-spreading viral outbreaks.
An optimised approach
Scientists at the NRC have developed a mammalian cell line that could be optimised for rapid antigen production. The research is expected to “majorly accelerate” the time needed for infectious disease vaccine development, says CEPI’s Executive Director of Manufacturing and Supply Chain (Acting), Ingrid Kromann.
“If successful, this optimised cell line could help vaccine doses be more rapidly available for clinical trials and initial emergency use during future outbreaks, supporting CEPI’s goal – embraced by Canada, and other G7 and G20 nations – to respond to a novel virus with a new vaccine in just 100 days after its discovery.”
Importantly, the technology is going to be suitable for transfer to low- and middle-income countries, enabling “local and rapid” vaccine production closer to the source of a future outbreak and improving accessibility. Dr Lakshmi Krishnan, Vice President of Life Sciences at the NRC, looks forward to working with CEPI to take the platform technologies forward to “accessible tools that could help accelerate vaccine production around the world”.
“Recognising the critical need for rapid vaccine production during a health emergency, this research and development project in our labs will advance innovative technologies to improve biomanufacturing processes and increase the efficiency of large-scale manufacturing of vaccines and other biologics.”
For the latest in vaccine technology for improved accessibility, join us at the Congress in Barcelona this month, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 16, 2024 | Technology |
A paper in Nature Biotechnology in October 2024 presents an “end-to-end clinical proteogenomic pipeline” to address the challenges associated with identification and prioritisation of antigenic peptides. NeoDisc combines “state-of-the-art publicly available and in-house software” with in silico tools to identify, predict, and prioritise tumour-specific and immunogenic antigens from multiple sources. The authors demonstrate the pipeline’s superiority over recent prioritisation pipelines and showcase the features that enable “both rule-based and machine-learning approaches”. They also reveal how NeoDisc’s multiomics integration identifies “defects in the cellular antigen presentation machinery”.
Antigen discovery
The researchers comment on the importance of personalised antigen discovery for the development of cancer vaccines. Common approaches for translational research and clinical trials include whole-genome sequencing (WGS) or whole-exome sequencing (WED) and RNA sequencing (RNAseq). However, the recent application of mass spectrometry (MS) to identify HLA-bound peptides and the use of proteogenomics have “facilitated the exploration of novel targets from a variety of antigens naturally processed and presented in cancer”.
“Their identification is laborious and current clinical pipelines do not support immunopeptidomics and are restricted to predicted neoantigens.”
Although immunotherapies are “remarkably effective” against some indications, “robust immune pressure” can force immune editing. Therefore, it is “essential” to understand the heterogenous antigenic landscape and the tumour’s capacity to present antigens.
The study
In the study, the authors introduce an “end-to-end” clinical antigen discovery proteogenomic pipeline: NeoDisc. It compiles publicly available and in-house software for the identification of immunogenic tumour-specific HLA-I and HLA-II antigens from genomics and transcriptomics and MS-based immunopeptidomics and enables their prediction and prioritisation with rule-based and machine-learning (ML) tools. It allows assessment of tumour heterogeneity and the functionality of the antigen processing and presentation machinery (APPM). The study compares NeoDisc’s performance with other tools, demonstrating its application for personalised antigen discovery and clinical implementation.
NeoDisc is a “dedicated computational framework” combining genomic, transcriptomic, and immunopeptidomic data and integrating curated public databases of known immunogenic TSAs, TAAs, oncoviral elements, and noncanonical transcripts. It uses matched tumour and germline genomic data for sample-specific variant characterisation, tumour content estimation, and copy number variation (CNV) and somatic mutation (SM) identification.
Four variant-calling algorithms are applied to WES and WGS data; variants that are detected by two or more callers are considered to have “high identification confidence”. Although highly mutated tumours usually respond better to immunotherapy, the selection of immunogenic neoantigens among “numerous possibilities” is “challenging”. Recent screening of large datasets of neoantigens in tumours from 112 participants has allowed the training of ML for prioritisation. ML classifiers trained on a fraction of this dataset have been integrated into NeoDisc to ensure “effective prioritisation”.
When NeoDisc’s rule-based and ML ranking approaches were compared with existing tools, the ML prioritisation algorithm “surpassed all the evaluated tools”. The researchers demonstrated NeoDisc’s “efficient prioritisation” on a cervical adenocarcinoma (CESC-1) characterised by an “exceptionally high mutational burden” (25 SMs per Mb).
Of the 393 identified actionable mutations, representing a pool of 19,051 peptides with a predicted binding rank ≤2%, 66 HLA-I neoantigenic short peptides (minimal epitopes) were selected through rule-based prioritisation for T cell screening of autologous tumour-infiltrating lymphocytes (TILs) by IFNγ ELISpot. 11 of the 66 peptides were immunogenic, including two that “ranked among the top ten candidates”. The NeoDisc ML model reordered the tested neoantigens, resulting in an “impressive” ranking of six immunogenic peptides in the top ten. NeoDisc also successfully identified two confirmed immunogenic neoantigens in the CESC-1 tumour MS immunopeptidomic data.
Personalised vaccines
While the default NeoDisc settings “exhibit good performance”, biopsies with low tumour content and low mutation burden could result in the detection of an “insufficient number of actionable high-confidence expressed mutations”. This would lead to a “suboptimal vaccine”. Thus, NeoDisc offers two additional modes:
- “Sensitive mode” considers the union of mutations called by all four variant-calling tools, to be used when an insufficient number of mutations are detected.
- “Panel mode” uses mutations listed in the available diagnostic clinical gene panel (GP) as input, allowing the design of vaccines for persons lacking dedicated biopsies. Note that GPs “often provide insufficient number of mutations leading to suboptimal lists of neoantigens or potentially none”.
The paper states that, in cancer vaccines, long sequences are favoured over minimal short peptides, motivated by the “efficient uptake and processing by APCs”. The NeoDisc ML tool ranks mutations according to their potential immunogenicity. Long sequences are “optimally” designed through maximised coverage of high-quality predicted HLA-I and HLA-II neoantigens.
In use in the field
NeoDisc is already being used in Phase I clinical trials for personalised cancer vaccines and adoptive T cell therapies in Switzerland; the authors hope that these demonstrate its “practical utility and potential for clinical translation”. Dr Michal Bassani-Sternberg of the Lausanne Branch of the Ludwig Institute for Cancer Research comments that NeoDisc provides “invaluable” insights into the immunobiology of tumours and the “mechanisms by which they evade targeting by cytotoxic T cells”.
“Notably, NeoDisc can also detect potential defects in the machinery of antigen presentation, alerting vaccine designers and clinicians to a key mechanism of immune evasion in tumours that can compromise the efficacy of immunotherapy. This can help them select patients for clinical studies who are likely to benefit from personalised immunotherapy, a capability that is also of great importance to optimising patient care.”
Florian Huber, first author, also reflected on the significance of this research.
“NeoDisc can detect all these distinct types of tumour-specific antigens along with neoantigens, apply machine learning and rule-based algorithms to prioritise those most likely to elicit a T cell response, and then use that information to design a personalised cancer vaccine for the relevant patient.”
Join us at the Congress in Barcelona this month to hear from experts in the Cancer and Therapeutic Vaccines track on their approaches to personalised vaccine development, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 15, 2024 | Technology |
In October 2024, Panthera Biopartners announced that Parexel has confirmed its inclusion in the Parexel Site Alliance Vaccine Network. Panthera becomes the first UK public or commercial clinical trial organisation to join the global network of high performing clinical trial sites. Parexel’s Site Alliance Vaccine Network “fosters long-term collaborative relationships” with research organisations across the globe to “deliver efficiencies”. Panthera was chosen to join the Network because of “exceptional performance in recruiting patients” across “numerous” studies and an existing “strong working relationship” with Parexel.
Patient recruitment
As the “UK’s largest recruiter and runner of commercial clinical trials across its UK sites”, Panthera has recently been the top recruiter globally in four studies, the top recruiter in the UK in six studies, and achieved first patient in globally or in the UK in nine studies. The company statement acknowledges that “less than 10%” of physicians and patients participate in clinical research. Among patients who do participate, “minority groups are significantly underrepresented”.
“Research activities are often concentrated in academic institutions and investigator sites, so patients and their providers are often unaware of the work, and even if they’re interested, many lack the time and resources required to join studies.”
Site Management Organisations (SMOs) like Panthera are focussed “entirely” on recruiting patients and running clinical trials, collaborating with local GP practices and using targeted advertising and social media campaigns to ensure that “all sections of the community” can participate.
Delivering efficiencies
The Parexel Site Alliance Network engages more than 340 sites and 16,000 investigators in “long-term collaborative relationships”. It is intended to “deliver efficiencies” to patients, sites, and customers. Members partner with Parexel to improve research and patient experiences.
Chris Dodd, Chief Commercial Officer at Panthera, described the company’s selection as a “testament to the effort we have put in to ensure we meet or exceed our patient recruitment targets”.
“We are delighted to be working in partnership with such a successful organisation with such great site communications and stakeholder management. We look forward to working together to bring even more clinical research to the UK.”
Join us at the Congress in Barcelona to explore ways in which the whole vaccine value chain can contribute to greater diversity in research and improved participant experiences. Don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 15, 2024 | Global Health |
A study in Emerging Infectious Diseases explores the association between COVID-19 vaccination and facial palsy (FP) in South Korea. The authors use an immunisation registry linked to the national health information database to compare FP incidence in a risk window with a control window. They found an increased FP risk within 28 postvaccination, primarily after first and second doses of both mRNA and viral vaccines. They encourage clinicians to “carefully assess” the FP risk-benefit profile associated with COVID-19 vaccines and monitor neurologic signs after vaccination.
Risk of facial palsy
Although no severe safety concerns were observed during the clinical trials of COVID-19 vaccines, an “imbalance” in facial palsy (FP) incidence after vaccination was identified in vaccinated persons compared to the general population. The aetiology of FP “remains elusive”, but autoimmune mechanisms or vaccination are “considered potential contributors to its development”. FP is included in the priority list of adverse events of special interest generated by the Safety Platform for Emergency vACcines (SPEAC) because of its “sudden and acute symptom onset”.
Despite multiple studies on the association of FP with COVID-19, we lack a “clear consensus”. As these studies have produced “controversial and inconclusive results”, the authors identified a need to generate an “in-depth body of evidence and a clear consensus” on the subject.
The study
The study uses two large, linked databases in South Korea to conduct a self-controlled case series analysis. It is intended to provide evidence on the safety of COVID-19 vaccines for immunisation under the COVID-19 Vaccine Safety Research Committee (CoVaSC) in South Korea. Several vaccines were available during the study period in South Korea:
- BNT162b2 (Pfizer-BioNTech)
- mRNA-1273 (Moderna)
- ChAdOx1 nCoV-19 (AstraZeneca)
- Ad.26.COV2.S (Janssen)
- NVX-CoV2373 (Novavax)
The researchers identified persons aged 18 and older who received an initial COVID-19 vaccine dose between 26th February 2021 and 1st March 2022. Among this population, they identified and included patients with a primary FP diagnosis accompanied by a prescription for corticosteroids between 26th February 2021 and 31st October 2022; patients who had received a COVID-19 vaccination and had incident FP diagnosed within a prespecified observation period were also included.
Exclusion criteria included foreign born residents, participants in clinical trials, persons vaccinated abroad, and persons deviating from vaccination guidelines to account for potential exposure misclassification. Persons with a history of FP in the year preceding the observation period and those whose FP cases occurred after the end of the observation period were excluded.
44,564,345 persons in South Korea were administered 129,956,027 COVID-19 vaccines doses between 26th February 2021 and 1st March 2022. During the study period, 15,472 FP cases with corticosteroid prescriptions were identified. Among these, 5,211 occurred up to 28 days postvaccination: 4.0 GP cases/1 million doses. Among the FP study population, the mean age at first COVID-19 vaccination was 53.1 years. 54.7% were male and 45.3% were female.
The study showed FP risk increased within 1-28 days after any COVID-19 vaccine dose. Increased FP risks were observed with the second dose and combined first and second doses, but no association was found for the third dose. The increased FP risk was identified across vaccine types. The incidence rate ratios (IRR) were “generally consistent” across age groups and, after application of the Benjamini-Hochberg adjustment, “generally remained consistent” across sex.
Implications
The findings of this study add to growing evidence of a positive association between FP and COVID-19 vaccination. The exact biological mechanism for the development of FP after vaccination remains unknown. However, “plausible links” between FP and mRNA and viral vector vaccines have been proposed. The study revealed increased FP risk in persons homologously vaccinated with mRNA vaccines, especially for BNT162b2 and in those with at least a single dose of mRNA vaccine. Furthermore, it revealed elevated risks among patients who received homologous dosing of viral vector vaccines.
An important consideration is the suggested link between COVID-19 infection itself and FP onset. In South Korea, the annual incidence of Bell’s palsy increased from 23.0 to 30.8 cases per 100,000 persons from 2008 and 2018. It reached 32.5 cases per 100,000 persons during 2021-2022, which suggests an increasing trend during the pandemic. Additionally, a study in South Korea indicated that COVID-19 infection is associated with a higher risk for Bell’s palsy for both COVID-19 vaccine recipients and nonrecipients.
“In conclusion, our study revealed a transient risk for FP after any dose of COVID-19 vaccine.”
The authors note that, although the risk for FP “appears elevated”, the absolute number of cases was “small”. Risk for FP should therefore not discourage patients from receiving COVID-19 vaccinations.
“Because FP is generally mild and manageable, physicians should monitor neurologic signs after COVID-19 vaccination and provide patients with a comprehensive evaluation of the risk-benefit profile associated with COVID-19 vaccines.”
Join us at the Congress in Barcelona this month to explore the processes by which vaccine safety is evaluated and monitored after rollout, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 14, 2024 | Global Health |
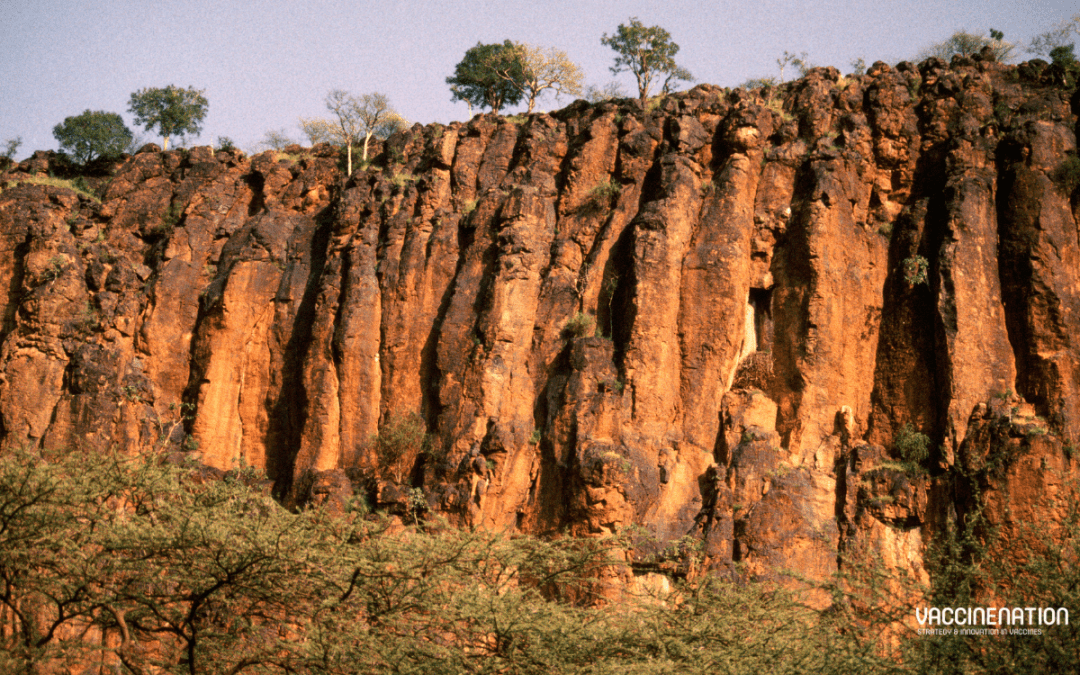
Phase II trials of a “promising” human vaccine candidate against Rift Valley fever are beginning in Kenya with CEPI support. CEPI reported in October 2024 that this is the “most advanced stage of testing” for a human Rift Valley fever vaccine in an “outbreak-prone area”. Scientists at the University of Oxford and the Kenya Medical Research Institute (KEMRI)-Wellcome Trust Research Programme are leading the trial with $3.7 million funding from CEPI.
Rift Valley fever
First identified in Kenya’s Rift Valley, Rift Valley fever is usually found in people after direct contact with infected animals or bites from infected mosquitoes. Most infected people experience “mild disease”, but a small proportion develop the “severe haemorrhagic form”, with a risk of blindness, convulsions, encephalitis, and bleeding. In these cases, mortality rates can reach 50%.
Rift Valley fever has been detected across “much of Africa” and in the Middle East. It is mosquito-borne, which makes it “climate sensitive”. There is therefore a risk of outbreaks spreading to new areas or increasing in frequency or size. There are Rift Valley fever vaccines for animals, but no currently available or licensed vaccines for human use; the disease is a priority disease for R&D for WHO and CEPI.
ChAdOx1 RVF in trial
The vaccine, known as ChAdOx1 RVF, is based on the University of Oxford’s ChAdOx1 vaccine platform. It has shown positive results in healthy adults in the UK, meeting “many of the optimal product characteristics” of a WHO target product profile. It is one of three Rift Valley fever candidates in CEPI’s portfolio. 240 healthy adults will participate in the research, following local trial approvals.
Funding for the trial comes under CEPI’s strategic partnership with the University to accelerate the development of globally accessible vaccines against outbreak pathogens. Both organisations are “committed to enabling access to any vaccine outputs developed through this partnership”, including developing a target product profile suitable for low- and middle-income countries (LMICs), assessing the need for technology transfer, and priority supply to LMICs at an affordable price.
Professor George Warimwe, Principal Investigator of the trail and Deputy Executive Director of the KEMRI-Wellcome Trust Research programme, reflected that “nearly 100 years” after the disease was identified, there are “still no approved vaccines or treatments”.
“This vaccine trial brings us closer to addressing the rising frequency of outbreaks.”
Dr Richard Hatchett, CEO of CEPI, commented that Rift Valley fever “disproportionately affects the lives and livelihoods of vulnerable pastoral communities”, causing human fatalities and livestock losses.
“Investing in the promising human ChAdOx1 RVF vaccine diversifies CEPI’s portfolio and gives us a greater chance at protecting vulnerable populations against this worrisome threat that may become more prevalent with climate change.”
Director General of Africa CDC, H.E. Dr Jean Kaseya, agreed that the disease “leads to livestock losses and human fatalities, thus impoverishing communities who largely depend on livestock for their livelihood”.
“The launch of a Phase II clinical trial of a Rift Valley fever vaccine candidate in an endemic country is a crucial milestone in our efforts to control this disease. Africa CDC is proud to support this initiative that not only prioritises the health of our people but also demonstrates the continent’s growing leadership in advancing clinical research.”
Dr Kaseya stated that the ChAdOx1 RVF vaccine “offers hope to vulnerable populations” who are “disproportionately affected by the growing impact of climate change”.
Join us at the Congress in Barcelona later this month to explore efforts to address the growing challenges of climate change and infectious disease with vaccine development and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 14, 2024 | Therapeutic |
Transgene announced in October 2024 that the primary objective of its randomised Phase II study of TG4001 has not been met. The study was evaluating TG4001 in combination with avelumab versus avelumab alone in patients with recurrent or metastatic HPV16-positive cervical and anogenital tumours. The primary objective was improvement in progression-free survival. Although this failure is “disappointing” to the company, Transgene states that it is evaluating the full results to “determine the best way forward”.
TG4001
Transgene’s TG4001 is an “innovative therapy capable of combating papillomavirus-induced cancers”. It teaches the immune system to identify and destroy the cancer cells expressing HPV-16 antigens, specifically E6 and E7.
Results and implications
The pre-planned subgroup analysis showed a positive efficacy trend in favour of the TG4001-containing regiment in cervical cancer patients. However, this requires further confirmation through additional analyses. These patients account for around half of the total patients enrolled in the study. Treatment was well tolerated, with adverse events “consistent” with previous observations.
“Transgene is currently evaluating the full study results in detail to determine the best way forward for this programme and will communicate further once this is completed.”
Dr Alessandro Riva, Chair and CEO of Transgene, acknowledged that “failure to meet the primary objective in our Phase II study with TG4001 is disappointing”.
“Nevertheless, we are encouraged by the positive efficacy trend in favour of the combination regiment in cervical cancer patients. We plan to complete a full and rigorous analysis of the data before deciding on any path forward for this asset.”
Dr Riva thanked patients and caregivers for their “important contribution” to the study.
“With a diversified portfolio of novel immunotherapies targeting solid tumours, our strategy remains focussed on advancing our lead asset, TG4050, an individualised cancer vaccine for head and neck cancers for use following surgery and adjuvant therapy.”
For the latest cancer vaccine research updates don’t forget to get your ticket to the Congress in Barcelona this month and subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 14, 2024 | Global Health |
In October 2024 the European Investment Bank (EIB Global) announced €2 million financing for early-stage vaccine development in Rwanda by Akagera Medicines Africa Limited. The support is intended to accelerate research, development, and manufacturing of new vaccines against infectious diseases like tuberculosis, HIV, Lassa fever, and Ebola. It will also be used to “strengthen technical skills and expertise” to support “home-grown discovery, manufacturing, and development of vaccine delivery systems” in Rwanda.
Global Gateway
This financing is part of the EU Global Gateway initiative, a strategy to “boost smart, clean, and secure links in digital, energy, and transport sectors and to strengthen health, education, and research systems”. Team Europe is mobilising up to €300 million between 2021 and 2027 to “allow EU’s partners to develop their societies and economies” whilst creating opportunities for EU Member States to “invest and remain competitive”. EIB Global supports “high impact investment” to enhance healthcare and pharmaceutical manufacturing, encourage greater “health resilience”, and support equitable access to healthcare.
Continent-based solutions
EIB Global states that Africa bears the highest disease burden globally, demanding “more home-grown or continent-based solutions”.
“Vaccination is a critical activity to ensure and guide investments in universal health and has a crucial role to play in achieving 14 of the 17 United Nations Sustainable Development Goals.”
Akagera Medicines was founded in 2018 and registered a 100%-owned subsidiary in Kigali in 2022. Its mission is “targeting tuberculosis and other infectious diseases with liposomal nanotherapeutics”. Commenting on the financing announcement at the World Health Summit in Berlin, Chief Executive Officer Michael Fairbanks recognised the “significant support” of the European Investment Bank.
“We are now a clinical company and moving faster to build human capacity and specialised infrastructure in Africa to support vaccine development.”
CEO of the Rwanda Social Security Board (RSSB) Regis Rugemanshuro stated that the financial support is an “important contribution to the realisation of Rwanda’s vision to become a biotech hub” and the wider vision of “Africa becoming self-reliant in vaccine and medicine manufacturing”.
“RSSB is looking forward to deepening partnerships with EIB and other international institutions to build resilient healthcare ecosystems in Rwanda and in Africa.”
Vice President of EIB Thomas Ostros identified the Bank’s “close cooperation with public and private partners” to “accelerate development of innovative solutions”.
“The EIB is committed to further strengthening our partnership with local and international players, to scale up investment and support innovative technology together.”
Belen Calvo Uyarra, EU Ambassador to Rwanda, agreed that the investment was another “important milestone”.
“Through Global Gateway, the EU is focussed on advancing equitable access to health products and local manufacturing in Africa.”
For more from key players in efforts to establish local manufacturing capacities in Africa and champions of equitable access to health products, join us at the Congress in Barcelona later this month. Don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 14, 2024 | Technology |
SK bioscience announced in October 2024 that it has signed an agreement to acquire a stake in Fina Biosolutions (FinaBio) with a $3 million investment. SK bioscience becomes FinaBio’s first and sole strategic investor with a goal of improving the immunogenicity and productivity of conjugate vaccines. This announcement is another example of SK bioscience’s investment in global companies to “create synergies in business” after recently completing the acquisition of a controlling stake in IDT Biologika. The company states that it is securing its “competitiveness” through strategic investments in “promising companies with exceptional technology” and M&As to “lay the foundation for a great leap forward into a leading global company”.
FinaBio’s technology
Founded in 2006, FinaBio seeks to “help emerging market vaccine manufacturers learn to make affordable protein polysaccharide conjugates for vaccines”. It is now a “premier provider” of laboratory and consulting services, specialising in the research and development of conjugate vaccines for pneumoniae, meningococcal, typhoid, and other diseases. One of FinaBio’s key assets is FinaXpress, a proprietary E. coli expression system, that can produce proteins not previously made in the bacteria, like the carrier protein CRM197. FinaBio has expanded access to this protein, marketed as EcoCRM.
FinaBio is also developing a next-generation conjugation technology that is site-specific and targets the desired location for antigen binding. This is intended to boost immunogenicity and productivity. Supplying conjugation technology and carrier proteins to various global biotech companies and institutions, FinaBio continues to expand its business units.
A conjugate collaboration
SK bioscience will use FinaBio’s CRM197 technology in its efforts to “secure the high effectiveness of diverse conjugate vaccines while increasing profitability through high-yield processes”. CEO and President of SK bioscience Jaeyong Ahn is “delighted to continue developing partnerships with global firms that have next-generation vaccine technology”.
“Through our mid- to long-term collaboration with FinaBio, we will advance the vaccines we are developing to the next level and strengthen our competitiveness for global market expansion.”
Dr Andrew Lees, Founder and CEO of FinaBio, apprecitaes SK’s “confidence” in the organisation and support of accelerated global commercialisation of EcoCRM.
“Combined with our efficient conjugation technology, this will enable the development of the next generation conjugate vaccines. It will also allow us to continue our mission of promoting affordable vaccines.”
We look forward to welcoming FinaBio back to the exhibition floor at the Congress in Barcelona later this month; get your tickets to connect with their team there and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 11, 2024 | Technology |
CEPI announced in October 2024 that the Centre for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota is to receive US$3.2 million to advance its open access Coronavirus Vaccines Research and Development (R&D) Roadmap. This is an “important tool created to guide the development of vaccines” against multiple coronaviruses. CIDRAP will monitor and evaluate R&D progress and “catalyse efforts” to develop broadly protective vaccines. The investment from CEPI will monitor progress towards the roadmap goals and milestones and enable the creation of an online database of current literature and reports on coronavirus vaccine research.
The CIDRAP roadmap
CIDRAP’s roadmap is developed with guidance from over 50 scientific leaders and financial support from The Rockefeller and Gates Foundations. It aims to respond to the threat of coronaviruses, highlighted in the experience of three new coronavirus epidemics (SARS, MERS, COVID-19) in just 20 years. Coronaviruses are a “real and present threat” that demand a “large, comprehensive, and coordinated” initiative.
“The ultimate goal of developing broadly protective coronavirus vaccines is therefore multi-faceted: to create more efficacious and durable COVID-19 vaccines, mitigate the potential threat of future coronaviruses that have not yet emerged, and, ideally, prevent infections and transmission.”
The roadmap covers five topic areas each with “key barriers and knowledge gaps” and corresponding “technical milestones for measuring success”:
- Virology applicable to vaccine R&D
- Immunology and immune correlates of protection
- Vaccinology
- Animal and human infection models for coronavirus vaccine research
- Policy and financing
CEPI’s support
The funding contributes to monitoring progress on these goals and milestones and supports an open access online research database as well as an open access online summary of all broadly protective coronavirus vaccines in preclinical and clinical development and a dashboard tracking funding and investment.
Dr Michael Osterholm, Regents Professor and Director of CIDRAP recognised CEPI’s contribution to coronavirus vaccine research and development.
“CEPI’s support and collaboration with CIDRAP will fast forward our efforts at creating broadly protective coronavirus vaccines.”
Dr Kent Kester, Executive Director of Vaccine R&D, CEPI, commented that COVID-19 was the “third new coronavirus to strike in the past 20 years, portending the emergence of further novel coronaviruses”.
“Having the latest information on vaccine research and progress within coronavirus vaccine R&D readily and openly available in CIDRAP’s roadmap will enhance the approach being pursued by CEPI and other scientific investigators around the world to develop vaccines that could confer protection against multiple coronaviruses at the same time.”
For the latest coronavirus vaccine research updates, including insights into the challenges of universal vaccine development, join us at the Congress in Barcelona this month. Don’t forget to subscribe to our weekly newsletters here.