by Charlotte Kilpatrick | Oct 24, 2024 | Technology |
The University of Connecticut (UConn) announced in October 2024 that associate Professor Thanh Nguyen’s research has received “significant” backing from The Bill and Melinda Gates Foundation. The Gates Foundation has awarded a series of grants totalling $6.6 million, following support from the National Institutes of Health (NIH) and the US Department of Agriculture (USDA). The funding will contribute to research and innovation for a microneedle array patch that can deliver multiple human vaccines at once. The Foundation initially awarded $2 million, which has increased after early success.
Microneedle array patch technology
Dr Thanh Nguyen works in the College of Engineering’s School of Mechanical, Aerospace, and Manufacturing Engineering. His microneedle method is “far less painful” than traditional syringe delivery and offers access and uptake benefits.
“What if we were able to mail people vaccines that don’t need refrigeration, and they could apply to their own skin like a bandage?”
The technology delivers highly concentrated vaccines in powder from over months, through a “nearly painless” 1-centimetre-square biodegradable patch.
“The primary argument is that getting vaccines and boosters is a pain. You have to go back two or three times to get these shots. With the microneedle platform, you put it on once, and it’s done.”
Funding increases
After the initial award of $2 million, the project made good progress and received additional funding to support the development of a scale-up manufacturing technology to produce patches on an industrial scale. In late September, the Gates Foundation awarded $4 million to take the patch “a step farther” as a pentavalent and Polio vaccine targeting diphtheria, tetanus, pertussis, HIV, Hepatitis B, and Polio. With this funding, the team can “build up productivity”. They are partnering with LTS to scale up production and are expanding the size of laboratory.
The award also marks a fundraising milestone for Dr Nguyen, who has earned more than $25 million in research awards, which he reflects “doesn’t come naturally”.
“It comes from the recognition of the high impact of the research and the lab’s success in publishing articles. It is a testament to the importance of what we are doing.”
For the latest vaccine development and technology updates, don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 23, 2024 | Technology |
The National Institute for Health and Care Research (NIHR) announced in October 2024 that the first Phase III randomised trial of an investigational mRNA norovirus vaccine is opening across the UK. The trial seeks to evaluate the efficacy and safety of mRNA-1403 and is sponsored by Moderna. It will be conducted across 39 sites in the country, including 27 NHS primary and secondary care sites. Investigators hope to recruit 2,500 participants between late October and early 2025.
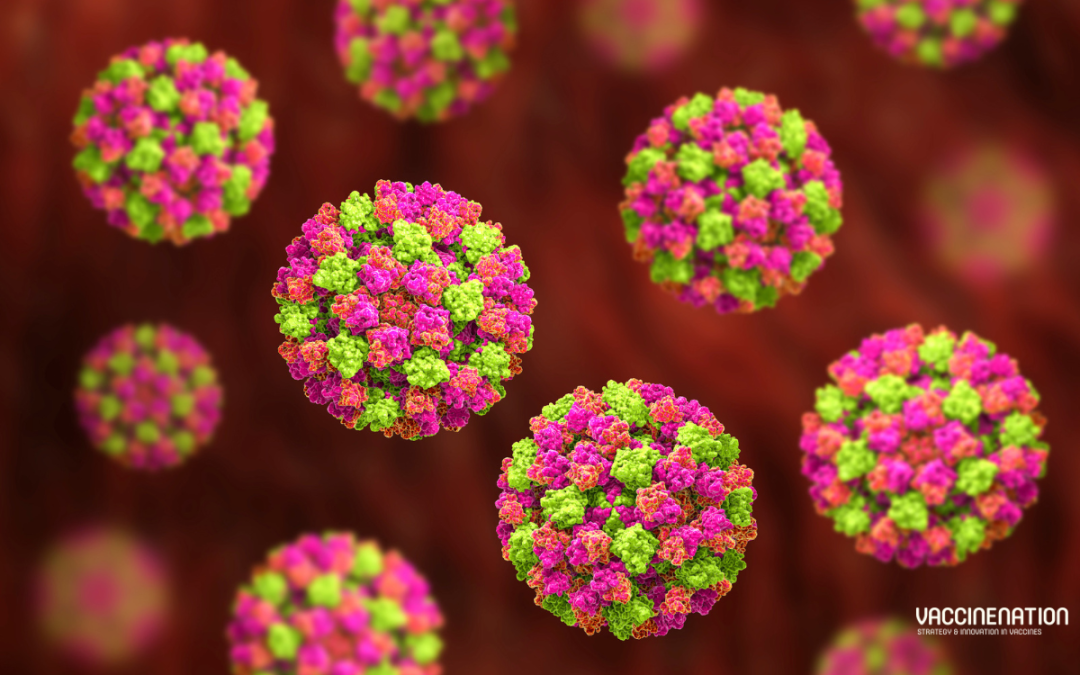
Norovirus
Norovirus, or the “winter vomiting bug”, is a viral illness; it is the “most common cause” of acute gastroenteritis globally. Symptoms include acute onset diarrhoea and vomiting, but there is evidence to suggest that norovirus infection is associated with intestinal inflammation and malnutrition and could cause long-term morbidity. WHO estimates that 685 million cases of norovirus are seen each year, including 200 million cases in children under 5.
“The burden of norovirus is significant; norovirus causes an estimated 200,000 deaths per year, including 50,000 child deaths, primarily impacting low-income countries. Norovirus has been estimated to cost $60 billion globally as a result of healthcare costs and economic losses.”
There are no licensed norovirus vaccines in use.
The trial
Participants in the trial will be randomly assigned to two groups. One group will receive the investigational vaccine, and the other groups will receive a placebo. While anyone who is aged 18 or older and meets the inclusion criteria is eligible for the trial, researchers are seeking participants aged 60 and older. This age group is “generally more likely to be severely affected by norovirus”. Thus, a successful vaccine would be of greatest benefit to them.
The trial is part of the 10-year partnership between Moderna and the UK Health Security Agency (UKHSA) on behalf of the UK Government. It is supported by the UK Vaccine Innovation Pathway (VIP) and the NIHR, which are working together to accelerate vaccine trials in the UK. The NIHR Research Delivery Network (RDN) is working with the devolved administrations to accelerate the roll-out of “key” vaccine studies. These efforts include the NIHR’s flagship recruitment tool: Be Part of Research.
Be Part of Research is an online service that connects people to health and care research across the UK. Anyone over the age of 18 can register for an account, indicating the areas of research that they are interested in. They are then sent information about suitable studies.
Advancing healthcare
The UK Chief Investigator, Dr Patrick, is a GP in Dorset and Research Director at the NIHR’s South West Regional Research Delivery Network. Dr Moore commented that the UK is “really pleased to be able to play an important role” in finding a vaccine for this “highly contagious disease”.
“Outbreaks of norovirus have huge consequences, both on our health systems and our economy. This innovative trial is crucial in helping us advance healthcare.”
NIHR Chief Executive and Chief Scientific Advisor to the Department of Health and Social Care, Professor Lucy Chappell, hopes that the vaccine could “make a difference to lives of many – especially our most vulnerable citizens”.
“Leveraging the UK’s expertise in vaccine development, the DHSC through the NIHR and Moderna are delivering this large-scale trial at pace, so that people across the UK and the world can benefit sooner.”
Health and Social Care Secretary Wes Streeting described the trial as a “huge vote of confidence in the UK’s life sciences sector”. It could also allow a “shift” away from sickness towards prevention, which would reduce pressure on the NHS and keep people healthier in the colder months. Moderna’s Chief Development Officer Dr Melanie Ivarsson is “delighted” to bring the trial to the UK.
“By advancing our investigational mRNA norovirus vaccine into a pivotal Phase III trial, we are one step closer to potentially providing a new tool to prevent infection from this highly contagious virus, which places a significant burden on health systems globally.”
Sarah Collins, Commercial Director at UKHSA, reflected that norovirus “isn’t just a nasty tummy bug – it can have serious consequences” including “disruption” to health services and education settings.
“It’s fantastic to see the first trial of its kind get underway as a result of UKHSA’s strategic 10-year partnership with Moderna, which aims to enhance investment in scientific research and vaccine development to enable a rapid response to future pandemics and other infectious diseases.”
For the latest on vaccine research, don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 18, 2024 | Technology |
In October 2024 the Animal and Plant Health Agency (APHA) and The Vaccine Group (TVG) announced that Innovate UK has awarded them a Smart grant in excess of £400,000 to advance a novel viral vector platform. In a project lasting 19 months, the two organisations will use technology developed by TVG scientists in candidate vaccines for two “important diseases in cattle”: bovine respiratory syncytial virus (BRSV) and lumpy skin disease (LSD). The project will continue previous research, which identified potential vaccine candidates; it is supported by the World Reference Laboratory for Non-Vesicular Diseases at The Pirbright Institute, determining how the candidates can produce an adequate serological response in animals and protect cattle.
BRSV and LSD
Bovine respiratory syncytial virus (BRSV) is the leading viral cause of respiratory illness in young calves in the UK. It affects around 1.9 million calves each year, costing approximately £54 million. It is “prevalent worldwide” and poses a “substantial economic burden” on beef and dairy producers. In the past 10 years, lumpy skin disease (LSD) has spread “dramatically” beyond former natural enzootic geographies in Africa and the Middle East to cause “severe disease” in other regions.
Both diseases have “broad global prevalence”, and BRSV particularly affects intensively reared cattle. Currently available commercial vaccines for BRSV do not prevent shedding and are restricted from use in young calves by maternal immunity. There are no DIVA (differentiating infected from vaccinated animals) vaccines available for LSD, so use is limited to areas where serosurveillance and eradication programmes are in place.
TVG’s vaccine solutions
The Vaccine Group (TVG) hope to address these challenges. With “key opinion leaders” for the two diseases in the UK and Canada, TVG has inserted transgenes for protective antigens from each virus into two separate constructs through genetic manipulation. Both vaccine candidates have been shown to be genetically stable and have demonstrated “stable and prolonged” protein expression in tissue culture over multiple passages. The technology works by introducing a benign virus to cattle, which stimulates the expression of proteins to induce an immune response.
Chief Executive Officer at TVG, Dr Jeremy Salt, reflected that infectious diseases are a “major cause for concern” for cattle farmers around the world, leading to “significant losses – both in terms of animal health and welfare, and in financial terms”.
“Our goal in developing a viral vector platform for use in cattle effective vaccines is to overcome some of the deficiencies that affect the current commercialised vaccines. By doing so, we can better protect the farmers, their animals, and their livelihoods.”
Dr Salt also hopes to “make beef and milk production more efficient, humane, and sustainable”, whilst “helping the sector address the global challenges of antibiotic resistance and carbon emissions”.
We look forward to hearing from Dr Salt at the Congress in Barcelona in just a few weeks; get your tickets to join us there and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 17, 2024 | Technology |
Valneva and LimmaTech Biologics announced in October 2024 that they have been granted Fast Track designation by the United States FDA for Shigella4V (S4V). S4V is “the world’s most clinically advanced” tetravalent bioconjugate shigellosis vaccine candidate. In August 2024 the two organisations announced a strategic partnership and exclusive licensing agreement to develop, manufacture, and commercialise S4V. The FDA designation is granted to products in development that have the potential to treat serious conditions and fill an unmet medical need, with the goal of facilitating clinical development and expediting review.
Addressing a global health threat
An estimated 165 million cases of disease and 600,000 deaths are attributed to Shigella every year; the greatest burden is among children in low- and middle-income countries (LMICs). Shigellosis also affects international travellers from high-income countries and deployed military personnel in endemic regions.
Thomas Lingelbach, Chief Executive Officer of Valneva, stated that shigellosis is the “second leading cause of fatal diarrhoeal disease worldwide” with no approved Shigella vaccine.
“The development of Shigella vaccines has been identified as a priority by the World Health Organisation (WHO). Fast Track designation allows us to work closely with the FDA to accelerate our efforts to deliver a preventative solution against this deadly disease.”
Dr Franz-Werner Haas, Chief Executive Officer of LimmaTech, is “highly encouraged” by the designation, which “reinforces our efforts”.
“[It] underscores the significant potential of the S4V Shigella vaccine candidate to address a serious global health threat.”
The way forward
After positive Phase I/II results earlier in the year, LimmaTech will conduct a Phase II Controlled Human Infection Model study (CHIM) in the United States and a Phase II paediatric study in LMICs. These are expected to begin before the end of 2024. Valneva will assume all further development, including chemistry, manufacturing, and controls (CMC) and regulatory activities. It will also be responsible for global commercialisation if the vaccine is approved.

by Charlotte Kilpatrick | Oct 16, 2024 | Technology |
CEPI announced in October 2024 that it is working with experts at the National Research Council of Canada (NRC) to bioengineer a “commonly used approach” to safely make protein antigens in “as little as two weeks”. This would be between eight and twelve times faster than the current timeline of antigen production for protein-based vaccines. CEPI is contributing up to CAD $850,000 and the NRC is providing up to CAD $308,000 (in kind) to establish proof-of-technology.
Low cost and high speed
CEPI notes the importance of manufacturers being able to make “sufficient quantities” of vaccine components at low cost to enable mass production. Although mammalian cell lines are a common choice for vaccine processes, boasting ease of culture and a high production yield, they can take four to six months to develop and optimise for antigen production. This is a “major challenge” to efforts to develop vaccines quickly in response to fast-spreading viral outbreaks.
An optimised approach
Scientists at the NRC have developed a mammalian cell line that could be optimised for rapid antigen production. The research is expected to “majorly accelerate” the time needed for infectious disease vaccine development, says CEPI’s Executive Director of Manufacturing and Supply Chain (Acting), Ingrid Kromann.
“If successful, this optimised cell line could help vaccine doses be more rapidly available for clinical trials and initial emergency use during future outbreaks, supporting CEPI’s goal – embraced by Canada, and other G7 and G20 nations – to respond to a novel virus with a new vaccine in just 100 days after its discovery.”
Importantly, the technology is going to be suitable for transfer to low- and middle-income countries, enabling “local and rapid” vaccine production closer to the source of a future outbreak and improving accessibility. Dr Lakshmi Krishnan, Vice President of Life Sciences at the NRC, looks forward to working with CEPI to take the platform technologies forward to “accessible tools that could help accelerate vaccine production around the world”.
“Recognising the critical need for rapid vaccine production during a health emergency, this research and development project in our labs will advance innovative technologies to improve biomanufacturing processes and increase the efficiency of large-scale manufacturing of vaccines and other biologics.”
For the latest in vaccine technology for improved accessibility, join us at the Congress in Barcelona this month, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 16, 2024 | Technology |
A paper in Nature Biotechnology in October 2024 presents an “end-to-end clinical proteogenomic pipeline” to address the challenges associated with identification and prioritisation of antigenic peptides. NeoDisc combines “state-of-the-art publicly available and in-house software” with in silico tools to identify, predict, and prioritise tumour-specific and immunogenic antigens from multiple sources. The authors demonstrate the pipeline’s superiority over recent prioritisation pipelines and showcase the features that enable “both rule-based and machine-learning approaches”. They also reveal how NeoDisc’s multiomics integration identifies “defects in the cellular antigen presentation machinery”.
Antigen discovery
The researchers comment on the importance of personalised antigen discovery for the development of cancer vaccines. Common approaches for translational research and clinical trials include whole-genome sequencing (WGS) or whole-exome sequencing (WED) and RNA sequencing (RNAseq). However, the recent application of mass spectrometry (MS) to identify HLA-bound peptides and the use of proteogenomics have “facilitated the exploration of novel targets from a variety of antigens naturally processed and presented in cancer”.
“Their identification is laborious and current clinical pipelines do not support immunopeptidomics and are restricted to predicted neoantigens.”
Although immunotherapies are “remarkably effective” against some indications, “robust immune pressure” can force immune editing. Therefore, it is “essential” to understand the heterogenous antigenic landscape and the tumour’s capacity to present antigens.
The study
In the study, the authors introduce an “end-to-end” clinical antigen discovery proteogenomic pipeline: NeoDisc. It compiles publicly available and in-house software for the identification of immunogenic tumour-specific HLA-I and HLA-II antigens from genomics and transcriptomics and MS-based immunopeptidomics and enables their prediction and prioritisation with rule-based and machine-learning (ML) tools. It allows assessment of tumour heterogeneity and the functionality of the antigen processing and presentation machinery (APPM). The study compares NeoDisc’s performance with other tools, demonstrating its application for personalised antigen discovery and clinical implementation.
NeoDisc is a “dedicated computational framework” combining genomic, transcriptomic, and immunopeptidomic data and integrating curated public databases of known immunogenic TSAs, TAAs, oncoviral elements, and noncanonical transcripts. It uses matched tumour and germline genomic data for sample-specific variant characterisation, tumour content estimation, and copy number variation (CNV) and somatic mutation (SM) identification.
Four variant-calling algorithms are applied to WES and WGS data; variants that are detected by two or more callers are considered to have “high identification confidence”. Although highly mutated tumours usually respond better to immunotherapy, the selection of immunogenic neoantigens among “numerous possibilities” is “challenging”. Recent screening of large datasets of neoantigens in tumours from 112 participants has allowed the training of ML for prioritisation. ML classifiers trained on a fraction of this dataset have been integrated into NeoDisc to ensure “effective prioritisation”.
When NeoDisc’s rule-based and ML ranking approaches were compared with existing tools, the ML prioritisation algorithm “surpassed all the evaluated tools”. The researchers demonstrated NeoDisc’s “efficient prioritisation” on a cervical adenocarcinoma (CESC-1) characterised by an “exceptionally high mutational burden” (25 SMs per Mb).
Of the 393 identified actionable mutations, representing a pool of 19,051 peptides with a predicted binding rank ≤2%, 66 HLA-I neoantigenic short peptides (minimal epitopes) were selected through rule-based prioritisation for T cell screening of autologous tumour-infiltrating lymphocytes (TILs) by IFNγ ELISpot. 11 of the 66 peptides were immunogenic, including two that “ranked among the top ten candidates”. The NeoDisc ML model reordered the tested neoantigens, resulting in an “impressive” ranking of six immunogenic peptides in the top ten. NeoDisc also successfully identified two confirmed immunogenic neoantigens in the CESC-1 tumour MS immunopeptidomic data.
Personalised vaccines
While the default NeoDisc settings “exhibit good performance”, biopsies with low tumour content and low mutation burden could result in the detection of an “insufficient number of actionable high-confidence expressed mutations”. This would lead to a “suboptimal vaccine”. Thus, NeoDisc offers two additional modes:
- “Sensitive mode” considers the union of mutations called by all four variant-calling tools, to be used when an insufficient number of mutations are detected.
- “Panel mode” uses mutations listed in the available diagnostic clinical gene panel (GP) as input, allowing the design of vaccines for persons lacking dedicated biopsies. Note that GPs “often provide insufficient number of mutations leading to suboptimal lists of neoantigens or potentially none”.
The paper states that, in cancer vaccines, long sequences are favoured over minimal short peptides, motivated by the “efficient uptake and processing by APCs”. The NeoDisc ML tool ranks mutations according to their potential immunogenicity. Long sequences are “optimally” designed through maximised coverage of high-quality predicted HLA-I and HLA-II neoantigens.
In use in the field
NeoDisc is already being used in Phase I clinical trials for personalised cancer vaccines and adoptive T cell therapies in Switzerland; the authors hope that these demonstrate its “practical utility and potential for clinical translation”. Dr Michal Bassani-Sternberg of the Lausanne Branch of the Ludwig Institute for Cancer Research comments that NeoDisc provides “invaluable” insights into the immunobiology of tumours and the “mechanisms by which they evade targeting by cytotoxic T cells”.
“Notably, NeoDisc can also detect potential defects in the machinery of antigen presentation, alerting vaccine designers and clinicians to a key mechanism of immune evasion in tumours that can compromise the efficacy of immunotherapy. This can help them select patients for clinical studies who are likely to benefit from personalised immunotherapy, a capability that is also of great importance to optimising patient care.”
Florian Huber, first author, also reflected on the significance of this research.
“NeoDisc can detect all these distinct types of tumour-specific antigens along with neoantigens, apply machine learning and rule-based algorithms to prioritise those most likely to elicit a T cell response, and then use that information to design a personalised cancer vaccine for the relevant patient.”
Join us at the Congress in Barcelona this month to hear from experts in the Cancer and Therapeutic Vaccines track on their approaches to personalised vaccine development, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 15, 2024 | Technology |
In October 2024, Panthera Biopartners announced that Parexel has confirmed its inclusion in the Parexel Site Alliance Vaccine Network. Panthera becomes the first UK public or commercial clinical trial organisation to join the global network of high performing clinical trial sites. Parexel’s Site Alliance Vaccine Network “fosters long-term collaborative relationships” with research organisations across the globe to “deliver efficiencies”. Panthera was chosen to join the Network because of “exceptional performance in recruiting patients” across “numerous” studies and an existing “strong working relationship” with Parexel.
Patient recruitment
As the “UK’s largest recruiter and runner of commercial clinical trials across its UK sites”, Panthera has recently been the top recruiter globally in four studies, the top recruiter in the UK in six studies, and achieved first patient in globally or in the UK in nine studies. The company statement acknowledges that “less than 10%” of physicians and patients participate in clinical research. Among patients who do participate, “minority groups are significantly underrepresented”.
“Research activities are often concentrated in academic institutions and investigator sites, so patients and their providers are often unaware of the work, and even if they’re interested, many lack the time and resources required to join studies.”
Site Management Organisations (SMOs) like Panthera are focussed “entirely” on recruiting patients and running clinical trials, collaborating with local GP practices and using targeted advertising and social media campaigns to ensure that “all sections of the community” can participate.
Delivering efficiencies
The Parexel Site Alliance Network engages more than 340 sites and 16,000 investigators in “long-term collaborative relationships”. It is intended to “deliver efficiencies” to patients, sites, and customers. Members partner with Parexel to improve research and patient experiences.
Chris Dodd, Chief Commercial Officer at Panthera, described the company’s selection as a “testament to the effort we have put in to ensure we meet or exceed our patient recruitment targets”.
“We are delighted to be working in partnership with such a successful organisation with such great site communications and stakeholder management. We look forward to working together to bring even more clinical research to the UK.”
Join us at the Congress in Barcelona to explore ways in which the whole vaccine value chain can contribute to greater diversity in research and improved participant experiences. Don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 14, 2024 | Technology |
SK bioscience announced in October 2024 that it has signed an agreement to acquire a stake in Fina Biosolutions (FinaBio) with a $3 million investment. SK bioscience becomes FinaBio’s first and sole strategic investor with a goal of improving the immunogenicity and productivity of conjugate vaccines. This announcement is another example of SK bioscience’s investment in global companies to “create synergies in business” after recently completing the acquisition of a controlling stake in IDT Biologika. The company states that it is securing its “competitiveness” through strategic investments in “promising companies with exceptional technology” and M&As to “lay the foundation for a great leap forward into a leading global company”.
FinaBio’s technology
Founded in 2006, FinaBio seeks to “help emerging market vaccine manufacturers learn to make affordable protein polysaccharide conjugates for vaccines”. It is now a “premier provider” of laboratory and consulting services, specialising in the research and development of conjugate vaccines for pneumoniae, meningococcal, typhoid, and other diseases. One of FinaBio’s key assets is FinaXpress, a proprietary E. coli expression system, that can produce proteins not previously made in the bacteria, like the carrier protein CRM197. FinaBio has expanded access to this protein, marketed as EcoCRM.
FinaBio is also developing a next-generation conjugation technology that is site-specific and targets the desired location for antigen binding. This is intended to boost immunogenicity and productivity. Supplying conjugation technology and carrier proteins to various global biotech companies and institutions, FinaBio continues to expand its business units.
A conjugate collaboration
SK bioscience will use FinaBio’s CRM197 technology in its efforts to “secure the high effectiveness of diverse conjugate vaccines while increasing profitability through high-yield processes”. CEO and President of SK bioscience Jaeyong Ahn is “delighted to continue developing partnerships with global firms that have next-generation vaccine technology”.
“Through our mid- to long-term collaboration with FinaBio, we will advance the vaccines we are developing to the next level and strengthen our competitiveness for global market expansion.”
Dr Andrew Lees, Founder and CEO of FinaBio, apprecitaes SK’s “confidence” in the organisation and support of accelerated global commercialisation of EcoCRM.
“Combined with our efficient conjugation technology, this will enable the development of the next generation conjugate vaccines. It will also allow us to continue our mission of promoting affordable vaccines.”
We look forward to welcoming FinaBio back to the exhibition floor at the Congress in Barcelona later this month; get your tickets to connect with their team there and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 11, 2024 | Technology |
CEPI announced in October 2024 that the Centre for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota is to receive US$3.2 million to advance its open access Coronavirus Vaccines Research and Development (R&D) Roadmap. This is an “important tool created to guide the development of vaccines” against multiple coronaviruses. CIDRAP will monitor and evaluate R&D progress and “catalyse efforts” to develop broadly protective vaccines. The investment from CEPI will monitor progress towards the roadmap goals and milestones and enable the creation of an online database of current literature and reports on coronavirus vaccine research.
The CIDRAP roadmap
CIDRAP’s roadmap is developed with guidance from over 50 scientific leaders and financial support from The Rockefeller and Gates Foundations. It aims to respond to the threat of coronaviruses, highlighted in the experience of three new coronavirus epidemics (SARS, MERS, COVID-19) in just 20 years. Coronaviruses are a “real and present threat” that demand a “large, comprehensive, and coordinated” initiative.
“The ultimate goal of developing broadly protective coronavirus vaccines is therefore multi-faceted: to create more efficacious and durable COVID-19 vaccines, mitigate the potential threat of future coronaviruses that have not yet emerged, and, ideally, prevent infections and transmission.”
The roadmap covers five topic areas each with “key barriers and knowledge gaps” and corresponding “technical milestones for measuring success”:
- Virology applicable to vaccine R&D
- Immunology and immune correlates of protection
- Vaccinology
- Animal and human infection models for coronavirus vaccine research
- Policy and financing
CEPI’s support
The funding contributes to monitoring progress on these goals and milestones and supports an open access online research database as well as an open access online summary of all broadly protective coronavirus vaccines in preclinical and clinical development and a dashboard tracking funding and investment.
Dr Michael Osterholm, Regents Professor and Director of CIDRAP recognised CEPI’s contribution to coronavirus vaccine research and development.
“CEPI’s support and collaboration with CIDRAP will fast forward our efforts at creating broadly protective coronavirus vaccines.”
Dr Kent Kester, Executive Director of Vaccine R&D, CEPI, commented that COVID-19 was the “third new coronavirus to strike in the past 20 years, portending the emergence of further novel coronaviruses”.
“Having the latest information on vaccine research and progress within coronavirus vaccine R&D readily and openly available in CIDRAP’s roadmap will enhance the approach being pursued by CEPI and other scientific investigators around the world to develop vaccines that could confer protection against multiple coronaviruses at the same time.”
For the latest coronavirus vaccine research updates, including insights into the challenges of universal vaccine development, join us at the Congress in Barcelona this month. Don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 11, 2024 | Technology |
Orlance, Inc., announced in October 2024 that it has been awarded a National Institutions of Health (NIH) Fast Track Small Business Innovation Research (SBIR) grant to develop an Enhanced Seasonal Influenza Vaccine that provides “better protection against disease” even in years when there is a mismatch between predicted and actual circulating strains. The award includes $300,000 for Phase I; the total funding for the Phase I and II combined programme amounts to $3.3 million. The grant enables Orlance to leverage its innovative MACH-1 powdered vaccine and immunotherapy platform to address both seasonally changing and highly conserved influenza immunogens.
MACH-1 for influenza
MACH-1 is a high-performance microparticle ‘gene gun’ technology that “efficiently and uniquely” delivers DNA or RNA vaccine-coated microparticles into cells in the epidermis, which is “rich in immune stimulating cells”. An advantage of this technology in comparison with currently licensed mRNA vaccines is that MACH-1-delivered vaccines are stable at room temperature and are painless and needle-free. These vaccines also offer protective levels of immunity with the “smallest doses yet achieved within the field”.
The grant will enable a project to address the limitations of current flu vaccines by broadening the number of influenza strains targeted in one vaccine. This means vaccine production can occur closer to influenza season and achieve a better match between predicted and actual circulating strains. It will also stimulate “more diverse types of immune responses” in systemic and localised cells. The programme builds on Orlance’s universal influenza vaccine, adding seasonally changing influenza antigens to maximise protection.
Excelling in the field
Orlance’s Head of Research and Development and Principal Investigator Dr Kenneth Bagley commented on the importance of the MACH-1 technology.
“The unique properties of MACH-1 delivery into the highly immune competent epidermis that generates potent systemic and local respiratory mucosal antibody- and T cell-mediate immunity, coupled with the large payload capacity of DNA vaccines, may allow for Orlance’s universal influenza vaccine to excel where other universal vaccines have failed.”
Kristyn Aalto, CEO of Orlance, recognised the “continued funding support” from NIH.
“[The] support of the MACH-1 platform including this enhanced seasonal influenza vaccine reinforces the potential impact and significant step forward MACH-1 can bring to vaccine technology.”
We welcome Kristyn to the Congress in Barcelona this month for the Mucosal and Alternative Delivery workshop; get your tickets to join us for this here, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 9, 2024 | Technology |
In October 2024, CEPI announced that it is awarding funding of up to £3.7 million to support researchers at the University of Sheffield as they seek proof-of-concept for RNAbox. RNAbox is a specialised process designed to scale up the production of mRNA vaccines at regional vaccine sites. It is “easily adaptable and automated”, with the potential to improve global pandemic readiness by enabling increased equitable access to various mRNA vaccines, as and when needed. It also could help speed up responses to future emerging outbreaks.
Addressing mRNA challenges
mRNA vaccines be “more rapidly tailored” to specific diseases or variants, and the technology “holds promise” for different illnesses, including emerging infectious diseases. However, mRNA vaccines are “expensive to manufacture at a high product quality” and require complex cold-chain storage and transportation infrastructure. This makes them “extremely difficult to deliver to remote areas or low-resource settings”.
The RNAbox presents a potential solution to these challenges through its bespoke manufacturing process, designed to overcome the need to deliver the vaccine by facilitating local manufacture at small production sites. The process will run continuously to create between seven and ten times more mRNA at a time and enable more efficient use of raw materials. RNAbox uses digital-twin technology, in which a virtual replica of the vaccine manufacturing process is modelled on a computer in real-time with smart sensors collecting data on the physical product.
CEPI’s interest
CEPI states that the “fast, optimised vaccine production is critical to the 100 Days Mission”. The investment will explore applying the technology to vaccine development for CEPI priority pathogens, including the viruses that cause deadly diseases like Ebola, Lassa fever, MERS, and Nipah. Ingrid Kromann, Acting Executive Director of Manufacturing and Supply Chain at CEPI suggested that the University’s “versatile” technology “builds on the ‘vaccine revolution’ experienced during the COVID-19 pandemic”.
“It aims to overcome a number of scientific hurdles which resulted in poorer countries facing devastating vaccine inequity by helping to make high-quality, low-cost vaccines quickly and easily close to the source of an outbreak.”
Dr Zoltán Kis, School of Chemical, Materials, and Biological Engineering at the University of Sheffield, reflected on the “importance of being prepared” with the “necessary tools”.
“We need to tackle outbreaks equitably around the world, as diseases can spread across country borders.”
The RNAbox will “accelerate the development of new vaccines” and “mass-manufacturing against a wide range of diseases”.
“This transformative technology can also be used to develop much-needed vaccines against a range of unmet needs during non-epidemic/pandemic times. In case of a new epidemic/pandemic, the RNAbox can be quickly adapted to produce vaccines to tackle outbreaks. This will enable vaccine development and manufacturing capacity locally in countries around the world to serve local needs.”
The researchers will work with vaccine manufacturers in low- and middle-income countries to ensure the technology is fit-for-purpose in lower-resource settings.
At the Congress in Barcelona this month we will hear from experts who are revolutionising mRNA vaccine production to ensure products are accessible. Join us there to learn more, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 7, 2024 | Technology |
In October 2024, WHO announced that a fourth WHO-prequalified human papillomavirus (HPV) vaccine product, Cecolin, has been confirmed for use in a single-dose schedule. This update is an “important milestone” that will contribute to “improving sustainable supply of HPV vaccines”, ensuring that more people get access to the vaccines that prevent cervical cancer. HPV vaccine programmes have been “hampered” by supply shortages since 2018, and recent production challenges have led to further shortfalls, which will affect girls in need of HPV vaccines Africa and Asia.
Eliminating cervical cancer by tackling HPV
More than 95% of the 660,000 annual cervical cases are caused by HPV. Every two minutes, a woman dies from the disease, and 90% of these deaths happen in low- and middle-income countries. 19 out of the 20 “hardest hit” countries are in Africa. However, vaccination is an effective way of addressing this health need. Dr Tedros Adhanom Ghebreyesus, WHO Director-General, states that “we have the ability to eliminate cervical cancer, along with its painful inequities”.
“By adding another option for a one-dose HPV vaccination schedule, we have taken another step closer in consigning cervical cancer to history.”
Dr Kate O’Brien, Director of the Department of Immunisation, Vaccines, and Biologicals at WHO, reflected that achieving a 90% coverage in girls by the age of 15 is the target of the first pillar of WHO’s global strategy for cervical cancer elimination.
“Given the continuing supply challenges, this addition of single dose vaccine product means countries will have greater choice of vaccines to reach more girls.”
Cecolin
Cecolin is a bivalent HPV vaccine delivered intramuscularly as a single dose. It is manufactured by Xiamen Innovax Biotech and should be stored between 2°C and 8°C. It is designed to protect against HPV types 16 and 18, which are commonly associated with the development of cancer. When Cecolin received prequalification, PATH stated that it had provided “technical assistance” for the process to facilitate greater accessibility. PATH’s China country representative Yuan Yuan commented that the vaccine would put the world “on its way to more equitable HPV vaccination”.
Single-dose coverage
Several products that were initially prequalified for use in a 2-dose schedule can now be used in a single-dose schedule. Cecolin can be recommended for “off-label” use after data support the modified schedule until the manufacturer adds the modified use to the label. Data from July 2024 show an increase in one dose HPV vaccine coverage among girls aged 9-14 years, from 20% in 2022 to 27% in 2023. In 2023, 37 countries were implementing a single-dose schedule; this increased to 57 by September 2024. WHO suggests that the adoption of a single-dose schedule has resulted in “at least” 6 million additional girls being reached with HPV vaccines in 2023.
For insights into the role of vaccination in elimination strategies, why not join us at the Congress in Barcelona this month? Don’t forget to subscribe to our weekly newsletters here for more vaccine news.

by Charlotte Kilpatrick | Oct 4, 2024 | Technology |
In September 2024, Vaxart announced the initiation of the sentinel cohort of its Phase IIb clinical trial evaluating the oral pill COVID-19 vaccine candidate in comparison with an approved mRNA vaccine. The funding is now approved for this part comprising 400 participants; 200 will receive Vaxart’s COVID-19 vaccine candidate and 200 will receive the approved mRNA vaccine comparator. The full trial will measure efficacy for symptomatic and asymptomatic disease, systemic and mucosal immune induction, and the incidence of adverse events.
Changing the vaccine landscape
Vaxart states that “for two hundred years vaccines have been administered by intramuscular injection”, offering the company’s oral pill vaccines as a way to “change everything”. The COVID-19 vaccine attacks invading pathogens at their points of entry, triggering strong IgA and T-cell responses to “repel and overwhelm” the invaders. It is designed to be stable at room temperature to allow global distribution with “wide public acceptance, minimal cost, and maximum speed”.
In trial
The Phase IIb trial has two parts and will enrol healthy adults in the United States. The first part will engage 400 participants; once an independent Data and Safety Monitoring Board (DSMB) and FDA review the data from these participants, the second part will be initiated, enrolling 10,000 participants. A goal of the trial is to enrol participants “in line with U.S. demographics”, and to include at least 25% over the age of 65.
The primary endpoint is relative efficacy of Vaxart’s candidate compared to the approved mRNA vaccine for the prevention of symptomatic disease. Primary efficacy analysis will be performed after all participants have either discontinued or completed a study visit 12 months after vaccination. Funding was granted through BARDA’s Project NextGen initiative to accelerate and streamline the development of innovative COVID-19 interventions, including vaccines.
A strong step
Dr James Cummings, Vaxart’s Chief Medical Officer, described the initiation of the sentinel cohort as a “strong step” towards the goal of “developing a vaccine that may bring us closer to a sustainable solution to the persistent threat of COVID-19″.
“We continue to progress toward our goal of conducting the Phase IIb study and look forward to the results of our mucosal technology’s first head-to-head comparison against an approved mRNA vaccine for this virus.”
We look forward to learning more about the vaccine’s progress from Dr Cummings at the Congress in Barcelona this month; if you’d like to join us there do get your tickets now. Don’t forget to subscribe to our weekly newsletters for more updates!

by Charlotte Kilpatrick | Oct 3, 2024 | Technology |
In October 2024, SK bioscience announced the successful completion of its acquisition of a controlling stake in IDT Biologika. This follows the announcement in June 2024 that SK bioscience intended to acquire 60% of IDT Biologika’s shares from the Klocke Group to “leap forward into global markets”. Since the signing of the sale and purchase agreement, SK bioscience has finalised the acquisition after obtaining the necessary approvals. The companies have established a plan for a post-merger integration (PMI) process of around 100 days. This will improve both companies’ “management effectiveness” and “encourage systematic integration for business growth”.
Building foundations
During the PMI, the companies will “build a foundation” for the growth of IDT Biologika through a series of projects. The first element seeks to maximise the utilisation rate of IDT Biologika’s manufacturing facilities and new capacities for drug substance (DS) and drug product (DP) for major projects with global pharmaceutical companies. SK bioscience also hopes to create a framework to expand existing contracts and win further projects for clinical trials and late-stage cell and gene therapy (CGT) projects. Alongside this, the portfolio of available cell lines will be expanded to address new customers, and the development of recombinant vaccines will be advanced.
SK biosciences will invest in high-growth businesses such as pre-filled syringes (PFS), recombinant vaccines, and CGT. This encompasses oncolytic virus (OV), adeno-associated virus (AAV), and lentivirus (LV). The company will also transfer technology and production to IDT Biologika for main products such as flu, shingles, chickenpox, and typhoid vaccines.
To “ensure synergies”, executives from both the Klocke Group and SK bioscience will serve on IDT Biologika’s Advisory Board. The Board will ensure “independent management while carrying out cultural integration”. Dr Ulrich Valley, CEO of IDT Biologika, is “convinced” that the milestone will “contribute to future growth and to our vision of a leading CDMO”.
“This global strategic cooperation is an important driver for our innovative strength, competitiveness, and sustainable success, built on a foundation of trust and common goals.”
Dr Valley is “certain” that Sk bioscience and IDT Biologika can “achieve great things together by combining our competences and capabilities”. President and CEO of SK bioscience, Jaeyong Ahn, commented that the with the successful completion of the acquisition, the two companies “now unite one family”.
“The capabilities and technologies of the two companies are expected to generate significant synergies, and we will accelerate our global expansion.”
We look forward to hearing from IDT Biologika on how to successfully scaling up for vaccine and CGT manufacturing at the Congress in Barcelona this month. Get your tickets to join us there, and don’t forget to subscribe to our newsletters for the latest vaccine news.

by Charlotte Kilpatrick | Sep 26, 2024 | Technology |
UNICEF announced in September 2024 that it is working with Australia and Samoa to improve access to vaccinations in Samoa. To this end, an innovative new vaccine delivery vehicle was delivered, alongside waste management supplies such as bins and masks. These supplies are intended for the benefit of everyone living in Samoa, including healthcare providers in 13 healthcare facilities.
A vehicular ‘boost’
UNICEF describes the arrival of the Pacific nation’s first vaccine delivery vehicle as a “boost” to the health system, with positive implications for cost effectiveness and wastage of resources for healthcare workers. Until this point, a smaller vehicle has been used to transport vaccines from the airport to the National Vaccine Centre, before distribution to health care facilities. This required more trips to ensure the potency and efficiency of the vaccines was maintained.
Although Samoa has been making “steady progress” in reaching eligible children with vaccines in the national immunisation schedule and has received support from UNICEF on cold chain and capacity building, the transportation and distribution of vaccines has been identified as a “gap”. The new vehicle, procured with support from the Australian Government and UNICEF, will enable faster transportation and can protect vaccines in unfavourable weather conditions.
Strengthening the health system
Samoa’s Hon. Minister of Health, Valasi Luapitofanua To’ogamaga Tafito Selesele, expressed gratitude to the Australian Government for “timely support” and UNICEF for “able technical guidance and support”, which will help to strengthen the health system to “get equipped to provide quality services in a cost-effective way”. Australia’s High Commissioner to Samoa, H.E. Will Robinson, stated that the vehicle, although prioritised for vaccines, can be used to “accommodate the pharmaceutical supplies for distribution” to health facilities.
“Australia is proud to be a long-term partner for Samoa in achieving its vision for a healthier community and delivering better health for all.”
UNICEF Pacific’s Chief of Samoa Field Office, Khin Moe Aye, recognised that “most” of the health issues facing children in Samoa and the Pacific are preventable.
“However, preventing them requires an effective primary healthcare system well-supported by sound resources. UNICEF is pleased to partner with the Australian Government and Ministry of Health in Samoa towards the strengthening of healthcare systems. This will enable children and their families to access quality services, while also ensuring that healthcare workers benefit from better resources and services.”
For the latest insights into strengthening healthcare systems and ensuring effective vaccine delivery strategies across the world, join us at the Congress in Barcelona next month. Don’t forget to subscribe to our weekly newsletters for more!

by Charlotte Kilpatrick | Sep 25, 2024 | Technology |
MSD Animal Health announced in September 2024 that it is expanding the newly USDA-approved NOBIVAC NXT vaccine platform to include a best-in-class solution to protect cats against a common feline infectious disease, feline leukaemia virus (FeLV). Describing this technology as a “breakthrough scientific achievement”, MSD Animal Health indicated that the vaccine is expected to be available at veterinary clinics and hospitals in the autumn.
NOBIVAC NXT
The NOBIVAC platform is behind a portfolio of products with an “extensive range of vaccines” to protect companion animals against various diseases. NOBIVAC NXT FeLV is the first and only feline leukaemia virus vaccine built using the RNA-particle technology platform. It is designed to deliver “optimised protection”. It is a nonadjuvanted, low volume 0.5 mL dose vaccine that “harnesses the natural ability of the immune system” to generate a robust response.
NOBIVAC NXT FeLV is labelled effective against persistent viraemia and is indicated for the vaccination of cats aged 8 weeks or older. The American Association of Feline Practitioners (AAFP) recommends administration in two doses, 3 to 4 weeks apart. It follows the AAFP’s recommendations for extended duration protection with a proven 2-year duration of immunity (DOI).
Feline leukaemia virus
Feline leukaemia virus can be spread in a “multitude of ways”, including mutual grooming, fighting behaviour, or shared food. It poses “serious” health risks, but cats often show no symptoms when they are first infected. However, as it persists, the virus can lead to cancer, severe blood disorders, or other infections associated with a compromised immune system. Routine vaccination can help protect from potential illness.
Meg Conlon, DVM, executive director, veterinary professional services, MSD Animal Health, suggested that “nearly 4% of cats” in North America are affected by the disease. This is a “notable percentage when there have been guidelines for prevention in place for decades”.
“That’s why education and awareness of the importance of vaccinating against this disease is so important.”
Ian Tarpey, vice president, research and development, MSD Animal Health, is proud to extend the RNA-particle technology with a vaccine that “protects against one of the most persistent threats to our feline patients”.
“MSD Animal Health and our NOBIVAC brand have a rich history in vaccine innovation, and we’re continuing to prove our dedication to ensuring there are safe and effective treatment options for veterinary professionals with the latest development of NOBIVAC NXT FeLV.”
For the latest on veterinary vaccines at the Congress in Barcelona next month, get your tickets to join us here and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Sep 23, 2024 | Technology |
Evaxion Biotech announced the launch of an enhanced version of its clinically validated AI-Immunology platform in September 2024, with an update to the EDEN AI prediction model. Improvements to the model include toxin antigen prediction, which enables the development of improved bacterial vaccines. AI-Immunology allows Evaxion to simulate the immune system and create predictive models to identify and develop personalised and other next-generation immunotherapies. It uses advanced AI and machine learning technologies to design and develop vaccine candidates in response to significant unmet needs.
EDEN upgraded
The AI-Immunology platform can deliver a new target within 24 hours, with “robustly validated” predictive capabilities. The EDEN prediction model is one of five models within the AI-Immunology platform. It rapidly identifies antigens that will trigger a robust protective immune response against “almost any” bacterial infectious disease. The model is fully AI-driven and designed to identify vaccine candidates “faster and at a lower cost than current state-of-the-art methods”. EDEN enables a novel approach to vaccine development that supports efforts against the “rising global issue of antibiotic resistance”.
The latest version 5.0 features several updates:
- Novel bacterial toxin antigen predictor – Evaxion has trained new machine learning models to improve the accuracy and reliability of toxin antigen prediction.
- Expanded training dataset – The process for curating additional training data from published sources has been streamlined with retrieval-augmented generation with large language models, followed by manual domain expert curation.
- Advanced protein feature prediction – The team has developed a new building block for protein feature prediction using protein language models, enhancing the model’s architecture and capability to predict various protein characteristics.
CEO of Evaxion, Christian Kanstrup, described the launch of the model as an “important milestone” that strengthens the AI-Immunology platform.
“As one of the few truly AI-first TechBio companies, our AI-Immunology platform is at the forefront of innovation. We wil continue to invest in its development and refinement to further improve our ability to discover novel targets and develop advanced vaccines.”
We look forward to learning more about the AI-Immunology platform at the Congress in Barcelona next month; get your tickets to join us there and don’t forget to subscribe to our weekly newsletters for more vaccine technology updates.

by Charlotte Kilpatrick | Sep 23, 2024 | Technology |
Vicebio announced $100 million Series B financing and the initiation of a Phase I clinical study of RSV/hMPV bivalent vaccine in September 2024. The financing is led by TCGX with investment from Goldman Sachs Alternatives, Avoro Ventures, and venBio, with participation from UniQuest and founding investor Medicxi. The funding will support and accelerate the development of vaccines based on Molecular Clamp technology, discovered at The University of Queensland.
Molecular Clamp technology
Vicebio’s next-generation vaccines for respiratory viruses are based on the proprietary Molecular Clamp technology from The University of Queensland. This technology “uniquely stabilises” viral glycoproteins in their immunogenic prefusion conformation, which is “crucial for eliciting strong protective immune responses”. The approach enables the production of “highly effective” vaccines that are easy to manufacture and can be available in ready-to-use prefilled syringes.
The technology has applications for a range of viruses, including respiratory syncytial virus (RSV), human metapneumovirus (hMPV), parainfluenza virus, influenza, and coronaviruses. This has been confirmed by “promising” preclinical and clinical studies.
Vicebio has recently initiated a Phase I clinical trial of VXB-241, a bivalent vaccine that targets both RSV and hMPV. These viruses cause a “significant burden of disease” in elderly patients and those with weakened immune systems. There is no commercially available vaccine for RSV and hMPV. The initial clinical readouts of the study are expected mid 2025.
Cutting-edge science
Dr Emmanuel Hanon, Chief Executive Officer of Vicebio, expressed enthusiasm for the latest interest.
“The support from these high-calibre investors underscores the robust data package we have generated for VXB-241, highlighting the significant potential of our proprietary Molecular Clamp technology to develop next-generation vaccines against respiratory viruses.”
Managing Partner at TCGX, Cariad Chester, emphasised TCGX’s dedication to supporting the “translation of cutting-edge science into transformative medicines”.
“We are thrilled to partner with Vicebio. This is a highly experienced team with a breakthrough technology to address a critical public health need. Vicebio has a unique capability to advance vaccine products that simultaneously provide robust immune responses against multiple respiratory pathogens.”
Cariad Chester will be included on the Vicebio Board of Directors and looks forward to working with the team to “bring these important vaccines to the market”. Dr Giovanni Mariggi, Chair of Vicebio and Partner at Medicxi, identified the “significant progress” Vicebio has made in developing the Molecular Clamp platform and advancing VXB-241 with “unmatched vaccine coverage”.
“We are pleased to welcome TCGX, Goldman Sachs, Avoro Ventures, and venBio to the syndicate to support the fight against life-threatening respiratory viral infections.”
For the latest vaccine technology insights at the Congress in Barcelona next month, get your tickets to join us here, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Sep 23, 2024 | Technology |
In September 2024 the United States FDA announced the approval of FluMist for self- or caregiver-administration. It is approved for active immunisation for the prevention of influenza disease caused by subtypes A and B in individuals aged 2 to 49. FluMist is administered as a nasal spray and was initially approved for use in 2003, with an expansion to include younger children in 2007. The latest approval was based on a submission that included results from a usability study, which demonstrated that individuals over the age of 18 could self-administer or administer FluMist to eligible recipients. It is the first vaccine to prevent influenza that does not require administration by a health care provider.
FluMist
The live attenuated influenza vaccine (LAIV) is administered as a nasal spray. The vaccine is recommended by the Advisory Committee on Immunisation Practices (ACIP) and American Academy of Paediatrics (AAP). A prescription is required to receive FluMist, but the vaccine can either be administered by a health care provider in a health care setting or by the vaccine recipient or caregiver over 18. Since its initial approval in the United States in 2003, almost 200 million doses have been distributed globally.
In FDA-required studies, AstraZeneca evaluated if individuals from 18 to 49 years of age could “appropriately” administer FluMist when given instructions. These studies showed that 100% of intended users administered a full dose, and that the efficacy, immunogenicity, and adverse events with self-administration were “similar to” those seen with administration in a health care setting.
The vaccine manufacturer will make the vaccine available through a third-party online pharmacy for people who are interested in self- or caregiver-administration. To order FluMist, these people will complete a screening and eligibility assessment before receiving a prescription and delivery of the vaccine. Individuals aged 2 to 17 should not self-administer.
Broader accessibility
Director of the FDA’s Centre for Biologics Evaluation and Research Dr Peter Marks commented that the approval provides a “new option” for safe and effective seasonal influenza vaccination, “potentially with greater convenience, flexibility, and accessibility for individuals and families”.
“Getting vaccinated each year is the best way to prevent influenza, which causes illness in a substantial proportion of the U.S. population every year and may result in serious complications, including hospitalisation and death. This approval adds another option for vaccination against influenza disease and demonstrates the FDA’s commitment to advancing public health.”
Dr Ravi Jhaveri, Division Head, Infectious Disease, Virginia H. Rogers Professor in Infectious Diseases, Professor of Paediatrics, Northwestern University School of Medicine, also emphasised the importance of increasing accessing to vaccinations to address the “significant burden” of influenza.
“For the first time, families and caregivers will be able to protect themselves against influenza with a needle-free, self-administered vaccine, from the convenience of their own home.”
Iskra Reic, Executive Vice President, Vaccines and Immune Therapies, AstraZeneca, stated that the approval of FluMist for self-administration is an “important step forward in making vaccines more accessible to fight the high annual burden of influenza”.
“For more than 20 years, FluMist has been the only nasal spray flu vaccine licensed in the US and now it is also the only vaccine to help individuals, families, and communities access an influenza vaccine conveniently through self- and caregiver-administration outside of traditional healthcare settings.”
To learn more about the various applications of nasal spray vaccines at the Congress in Barcelona next month, get your tickets to join us here. Don’t forget to subscribe to our weekly newsletter for more vaccine insights.

by Charlotte Kilpatrick | Sep 19, 2024 | Technology |
An article in Scientific Reports in September 2024 uses Digital Shadows to facilitate a comparison of recombinant DNA and in vitro (IVT) mRNA vaccine manufacturing technologies. The authors offer an assessment of which manufacturing platform is better suited for two types of vaccines. They suggest that recombinant DNA technology exhibits a higher Profitability Index, but mRNA offers faster high potency in short product development cycles.
Technical and economic benefits
Limitations in “traditional vaccines” have “speared” the development of novel technologies for antigens and monoclonal antibodies, including the recent use of recombinant DNA and RNA technologies in the COVID-19 pandemic. Recombinant DNA technology requires the insertion of a gene encoding the relevant pathogen or immunoglobulin sequence into a cell factory organism, which produces the antigen or antibody. RNA technology uses stoichiometric biochemical reactions to produce mRNA (messenger RNA) encoding the antigen or antibody, which is translated in vivo by the recipient’s cells.
Both mRNA and DNA technologies have “established proof of therapeutic effectiveness”. However, they differ in approach to obtaining the therapeutic protein of choice, which leads to different manufacturing processes. For recombinant DNA, the process is “time-consuming and expensive, requiring specialised laboratory facilities and trained personnel”. By contrast, IVT mRNA is understood to be “fast, flexible, and inexpensive”. This is offset by the need for cold transportation and storage to cater to the “instability and sensitivity” of the RNA molecule. Furthermore, IVT mRNA-based vaccine manufacturing has not been standardised.
Both technologies have “captured the global scientific interest” and present opportunities in the treatment of cancer and autoimmune diseases among others. However, the authors state that that there is no comparison of the two technologies on technical and economic levels.
The study
Digital Shadows are “enabling tools suitable to model a system in a fiat cyber-physical environment, delivering data flow abstractions of processing performance”. They are also used in the study to simulate and analyse the “technical merits and production costs” of each technology at given operating conditions. This allows the researchers to investigate root cause deviations and evaluate the cost-effectiveness scenarios of each proposed solution.
The authors constructed Digital Shadows to compare recombinant manufacturing of monoclonal antibodies and antigens with IVT mRNA production processes. They developed algorithmic threads to explore strengths and weaknesses, offering “enabling tools of strategic decision planning”.
The research suggests that recombinant production methods create “highly stable and therefore advantageous products”, with a proven track record of clinical safety and efficacy, and a low risk of unknown side effects, carrier-related allergic reactions, and withdrawals. The vaccines require “minimal maintenance” to preserve stability and functionality, which “ameliorates any respective logistical challenges and minimises the risks related to post-production regulatory withdrawals”. The components needed for production are “accessible” for the pharmaceutical industry but may come under pressure in case of pandemic outbreaks.
A drawback of the recombinant DNA vaccine production platform is its “complicated and therefore difficult-to-automate sub-processes”. The technology requires additional personnel for “process supervision and control purposes”. The platform is therefore “less appropriate for encountering pandemic bursts” or tracking mutations.
Another concern is the high risk of material contamination in cellular protein production, particularly in upstream processing. If contamination occurs, the cell line and its products are discarded, which causes delays and financial losses. Alongside this risk, recombinant DNA and protein production methods feature “low production yield”, which means that raw and side materials are purchased at high quantities and handled by expert personnel to reach the necessary production capacity.
IVT mRNA manufacturing protocols have “strong competitive advantages” in some characteristics. Although the vaccine is “highly sensitive to environmental conditions”, the production process is “easier to standardise, automate, adapt, and operate in continuous mode” thanks to the synthetic chemical nature of its sub-processes. The biochemical section of related processes can offer a “less complex, more effective” alternative with minimal requirements. This reduces the risks of cross contamination and quality-related batch rejections, producing higher yields and limiting product losses; it also lowers raw material processing resources and reduces development time.
Conclusions
For monoclonal antibody products, the study showed that recombinant DNA technology had a higher Profitability Index than IVT mRNA manufacturing. While the recombinant DNA monoclonal antibodies require a significantly higher dose due to an inferior potency profile, this is not reflected analogously in the final production cost. IVT mRNA manufacturing also had “higher dependencies” on raw materials.
When considering antigenic vaccines, the authors found that recombinant DNA technology demonstrated “higher economic performance”, demanding reduced capital resources. It also encompasses “proven, well-grounded protocols” for process development. Recombinant manufacturing “appears advantageous” by meeting technical and financial expectations. However, IVT mRNA “significantly” shortens the timeline from development to clinical application and benchtop to scale manufacturing. It also offers “unparalleled advantages” in synthetic processes and reduced requirements for installing large-scale production equipment.
The paper concludes that clinical trials and field practice will reveal if mRNA technologies can offer non-inferior therapeutic results compared to their DNA recombinant established alternatives. If you have worked with either of these technologies, what are your impressions or predictions? Why not join us at the Congress in Barcelona next month to share your insights into various platform technologies, and don’t forget to subscribe to our weekly newsletters for the latest vaccine news.