by Charlotte Kilpatrick | Oct 21, 2024 | Therapeutic |
Research in Nature in October 2024 leverages evidence that bacteria “naturally home in on tumours and modulate antitumour immunity” to explore potential vaccine applications. The authors engineered a probiotic Escherichia coli Nissle 1917as an antitumour vaccination platform, revealing a promising immune response. In mouse models of advanced colorectal cancer and melanoma, the vaccine triggered the immune system to suppress the growth of primary and metastatic cancers. The team hopes that this research can advance personalised cancer vaccine approaches.
Bacteria as ideal vectors
The authors identified bacteria as “ideal vectors to augment and direct” antitumour immune responses thanks to their support of the activation of both innate and adaptive immunity. Furthermore, bacteria can be synthetically engineered with ease for “safe delivery” of immunomodulatory compounds. Although various tumour neoantigen vaccines have demonstrated “promising” clinical trial results, benefit is “limited to only a subset of patients”. Thus, programming bacteria with genetic directives to release high levels of specific tumour neoantigens offers a system for the precise instruction of neoantigen targeting in situ.
The study
The researchers developed an engineered bacterial system in probiotic Escherichia coli Nissle 1917 (EcN) to “enhance expression, delivery, and immune-targeting of arrays of tumour exonic mutation-derived epitopes”. These epitopes are “highly expressed” by tumour cells and predicted to bind major histocompatibility complex (MHC) class I and class II. The system engages several “key design elements” to enhance therapeutic use:
- Optimisation of synthetic neoantigen construct form with
- Removal of cryptic plasmids and deletion of Lon and OmpT proteases to increase neoantigen accumulation
- Increased susceptibility to phagocytosis for enhanced uptake by antigen-presenting cells (APCs) and presentation of MHC class II-restricted antigens
- Expression of listeriolysin O (LLO) to induce cytosolic entry for presentation of recombinant encoded neoantigens by MHC class I molecules and T helper 1 cell (T H1)-type immunity
- Improved safety for systemic administration due to reduced survival in the blood and biofilm formation
Through exome and transcriptome sequencing of subcutaneous CT26 tumours the researchers developed a repertoire of neoantigens, which were predicted from highly expressed tumour-specific mutations. They then endeavoured to create a microbial system that could “accommodate the production and delivery of diverse sets of neoantigens” to lymphoid tissue and the tumour microenvironment (TME).
“Synthetic neoantigen construct optimisation and genetic engineering achieved a microbial platform (EcNcΔlon/ΔompT/LLO+) capable of robust production across diverse sets of tumour neoantigens, which was attenuated in immune-resistance mechanisms, effectively taken up by and proficient in activating APCs, and able to drive potent activation of T cells specific for encoded recombinant antigens to support enhanced cellular immunity.”
Vaccine applications
The study revealed that antigen sets encompassing predicted MHC-II and MHC-II binding neoantigens mediated antitumour efficacy. Enhanced frequencies of neoantigen-specific CD4+ and CD8+ T cells were seen. Across distinct tumour models and genetic backgrounds, the antitumour effect of vaccination was “accompanied by broad modulation of the immune compartment within the TME”.
“The coordinated regulation of APCs, reduction of immunosuppressive myeloid, regulatory T and B cell populations, and activation of NK cells and CD4+ and CD8+ T cells together indicate the advantage of precisely engineered microbial platforms as next-generation antitumour vaccines that align several arms of immunity.”
Furthermore, the “unique ability” of microbial vaccines to “directly remodel” the TME could “promote synergy” across various forms of immunotherapy. Microbial neoantigen vectors locally increase neoantigens density, recruit and activate dendritic cells and CD4+ and CD8+ T cells, and reduce immunosuppressive populations and ligands within the TME. Therefore, in combination with adoptive T cell therapy (ACT), they could “oppose these resistance mechanisms and provide synergistic benefit”.
“Through extra programming of the microbial vectors and rational incorporation of other immunotherapeutics, this system may achieve reliable eradication of established solid tumours and metastases through precision cancer immunotherapy using living antitumour vaccines.”
Getting closer
Jongwon Im, PhD student at Columbia University, helped lead bacterial engineering aspects of the study, and commented on the “net effect”.
“The bacterial vaccine is able to control or eliminate the growth of advanced primary or metastatic tumours and extend survival in mouse models.”
These vaccines are personal, programmed to “direct the immune system” to target “distinct genetic mutations”, said Dr Nicholas Arpaia, associate professor of microbiology and immunology at Columbia University’s Vagelos College of Physicians and Surgeons.
“As we continue to integrate additional safety optimisations through further genetic programming, we are getting closer to the point of testing this therapy in patients.”
Dr Tal Danino, associate professor of biomedical engineering at Columbia’s School of Engineering, reflected that the time to treatment will “first depend on how long it takes to sequence the tumour” for each patient.
“Then we just need to make the bacterial strains, which can be quite fast. Bacteria can be simpler to manufacture than some other vaccine platforms.”
Another benefit of bacteria is the enabled delivery of a “higher concentration of drugs that can be tolerated when these compounds are delivered systemically throughout the entire body”, suggested Dr Arpaia.
“Here, we can confine delivery directly to the tumour and locally modulate how we’re stimulating the immune system.”
For the latest insights into cancer vaccine research make sure you join us at the Congress in Barcelona next week, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 14, 2024 | Therapeutic |
Transgene announced in October 2024 that the primary objective of its randomised Phase II study of TG4001 has not been met. The study was evaluating TG4001 in combination with avelumab versus avelumab alone in patients with recurrent or metastatic HPV16-positive cervical and anogenital tumours. The primary objective was improvement in progression-free survival. Although this failure is “disappointing” to the company, Transgene states that it is evaluating the full results to “determine the best way forward”.
TG4001
Transgene’s TG4001 is an “innovative therapy capable of combating papillomavirus-induced cancers”. It teaches the immune system to identify and destroy the cancer cells expressing HPV-16 antigens, specifically E6 and E7.
Results and implications
The pre-planned subgroup analysis showed a positive efficacy trend in favour of the TG4001-containing regiment in cervical cancer patients. However, this requires further confirmation through additional analyses. These patients account for around half of the total patients enrolled in the study. Treatment was well tolerated, with adverse events “consistent” with previous observations.
“Transgene is currently evaluating the full study results in detail to determine the best way forward for this programme and will communicate further once this is completed.”
Dr Alessandro Riva, Chair and CEO of Transgene, acknowledged that “failure to meet the primary objective in our Phase II study with TG4001 is disappointing”.
“Nevertheless, we are encouraged by the positive efficacy trend in favour of the combination regiment in cervical cancer patients. We plan to complete a full and rigorous analysis of the data before deciding on any path forward for this asset.”
Dr Riva thanked patients and caregivers for their “important contribution” to the study.
“With a diversified portfolio of novel immunotherapies targeting solid tumours, our strategy remains focussed on advancing our lead asset, TG4050, an individualised cancer vaccine for head and neck cancers for use following surgery and adjuvant therapy.”
For the latest cancer vaccine research updates don’t forget to get your ticket to the Congress in Barcelona this month and subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 8, 2024 | Therapeutic |
A study in the Journal for ImmunoTherapy of Cancer finds that vaccination in a clinically relevant genetic cancer mouse model generated a population of functional progenitor tumour-specific CD8 T cells (TST) and halted cancer progression, in contrast to immune checkpoint blockade (IBT) therapies. The authors hope that immunisation could be the “most effective strategy” for patients with early cancers or at high risk of cancer recurrence. This study takes a different approach to many cancer vaccine studies, which tend to focus on patients with advanced tumours.
Cancer vaccine potential
The authors recognise the transformational role of immunotherapies in the cancer treatment landscape, particularly in the case of immune checkpoint blockade (ICB). However, vaccines for non-viral cancers have had “more limited success”. Many studies on tumour-specific CD8 T cell (TST) vaccine responses are conducted in the established/late tumour setting, so less is known about how TST “respond and differentiate” in response to immunotherapy during early stages of tumorigenesis.
Previously, the authors developed an autochthonous mouse model of liver cancer (AST;Cre-ERT2) to initiate liver carcinogenesis with tamoxifen (TAM)-induced Cre-mediated SV40 large T antigen (TAG) expression in hepatocytes. TAG functions as an oncogene and a tumour-specific neoantigen recognised by CD8 T cells, so the model enables “precise temporal control” of the duration of TST interactions with transformed hepatocytes and tumours. In contrast to human tumours, which “arise sporadically and progress clonally”, TAM-induced oncogene induction is “highly efficient”, resulting in high antigen burden even at early stages.
The study
The researchers allowed AST;Cre-ERT2 mice to undergo stochastic TAG oncogene activation through sporadic, TAM-independent Cre-mediated activity. To explore TST responses against TAG-driven tumours they used congenic donor lymphocytes from transgenic mice, in which CD8 T cells express a single T cell receptor (TCR) specific for TAG epitope-I (TCRTAG). They found that TST became dysfunctional in TAM-treated AST;Cre-ERT2 mice and were “unable to halt tumour progression”. TAM-treated AST;Cre-ERT2 mice had a “substantial” tumour antigen burden, even at early stages of tumorigenesis.
To compare initial TST differentiation in mice with early liver lesions against those with late liver lesions, the researchers transferred CFSE-labelled naïve TCRTAG into early and late time point AST;Cre-ERT2 mice. TCRTAG in mice with early lesions divided at a slower rate, particularly in the spleen and ldLN, and there were fewer TCRTAG in the spleens, ldLN, and livers of early mice. Decreased TST proliferation in mice with early lesions could be due to the lower TAG antigen burden. Although nearly all TCRTAG in mice with late lesions and most in mice with early lesions failed to produce effector cytokines TNFα and IFNγ within 60 hours of transfer, a population of TCRTAG in were identified in the spleen and liver of mice with early lesions. These could produce effector cytokines TNFα and IFNγ.
“Thus, in hosts with sporadic early lesions, a subset of TST resisted rapid differentiation to the dysfunctional state, raising the possibility that this subset might be amenable to immunotherapeutic reprogramming/rescue.”
To see if this functional TST subset persisted, the authors examined TCRTAG immunophenotype and function 5 days and 21 days post-transfer into early or late AST;Cre-ERT2 mice. While fewer TCRTAG were found in mice with early lesions compared to late lesions at 5 days, the difference became less pronounced at 21 days. In both groups TCRTAG upregulated CD44, which indicates antigen exposure and activation. TCRTAG in early mice continued to express higher levels of PD1 than naïve TCRTAG, suggesting that PD1 expression can identify tumour-reactive TST in hosts with early lesions.
The next consideration was if the functional TST subset in mice with early lesions could be harnessed to stop tumour progression. LM, a gram-positive intracellular bacterium, induces strong CD4 and CD8 T cell responses. The researchers used an actA inIB deficient attenuated LM vaccination strain to test if early vaccination of AST;Cre-ERT2 would protect mice against liver cancer progression. Mice were either left untreated, given a single dose of empty LM, or vaccinated with a single dose of LM- TAG.
“LM- TAG–immunisation conferred a major survival advantage, with all mice remaining tumour-free and one mouse euthanised for dermatitis without any evidence of liver tumours.”
The mice in untreated and empty LM groups reached endpoint with “multiple” large liver tumours and increased liver weight. At endpoint, most TCRTAG in the LM- TAG–immunised made effector cytokines, in contrast to the TCRTAG in tumour-bearing mice in the other groups, which were “largely unable to produce effector cytokines”.
Vaccination vs ICB
“An important and open question in cancer immunotherapy is how ICB versus vaccination compares in boosting anticancer immune responses, and how best to combine and sequence these therapies.”
A comparison of ICB, LMTAG vaccination, and combined ICB/LMTAG vaccination found that ICB conferred no benefit in comparison with isotype control antibodies (iso). By contrast, LMTAG and ICB/LMTAG treated mice had no evidence of tumour progression at 400+ days. Furthermore, LMTAG vaccination, whether alone or in combination, led to a “substantial increase” in TST numbers and IFNγ production, while ICB alone had “little impact”.
LM-based vaccines have had “poor or mixed results” in clinical trials, often with a target of patients with advanced or refractory cancers. The authors hope that their studies offer “mechanistic insight” as to why these fail in patients with advanced cancers: “for vaccines to be effective, a progenitor TST population must be present”. Although the apparent superiority of vaccination over ICB “may be surprising at first glance”, the authors highlight an important point, that “not all TCF1+TST are functional, nor does ICB alone lead to functional TST”. However, the findings suggest that LMTAG vaccination maintains or rescues functional progenitor TCF1+TST.
Timing is important
Dr Mary Philip, associate director of the Vanderbilt Institute for Infection, Immunology, and Inflammation, commented that the study “suggests that the timing of vaccination is important”.
“A unique feature of our study is that these mice are at high, essentially 100% risk of developing cancers, so the fact that a single immunisation at the right time can give lifelong protection is pretty striking.”
Dr Philip reflected that very few studies follow mice “so long after vaccination” and find them tumour free for two years.
“ICB works by taking the brakes off T cells, but if the T cells have never been properly activated, they are like cars without gas, and ICB doesn’t work. The vaccination boosts the T cells into a functional state so that they can eliminate early cancer cells.”
For more progress updates from cancer vaccine researchers at the Congress in Barcelona this month, get your tickets to join us here. Don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Oct 2, 2024 | Therapeutic |
Interim Phase II data from Gritstone bio’s study evaluating GRANITE in September 2024 are described as “encouraging” in a company statement. The study evaluates Gritstone’s individualised neoantigen targeting immunotherapy in frontline microsatellite stable colorectal cancer (MSS-CRC) as maintenance therapy in combination with immune checkpoint inhibitors and fluoropyrimidine/bevacizumab. These data show the vaccine’s potential to extend progression-free and overall survival, but “fell short” of the target that some suggest is needed to “transform its fortunes”.
Encouraging data
104 patients were randomised 1:1 in the study, and the treated analysis shared by Gritstone includes 69 patients. Highlights from the data include:
- An emerging progression-free survival (PFS) benefit to all GRANITE recipients
- 21% relative risk reduction of progression or death with GRANITE compared to standard of care (SOC) control in all treated population
- 33% of GRANITE and 23% of control patients remain on study and free of progression
- Clinical benefit was most notable in patients with low disease burden (defined as patients with circulating tumour DNA (ctDNA) equal to or below the trial population median value at study entry)
- 38% relative risk reduction of progression or death with GRANITE compared to SOC control with low ctDNA subgroup
- Low baseline ctDNA is a likely prognostic and predictive factor
- Immune data were consistent with clinical activity
- Functional neoantigen-specific T cells observed in all 16/16 GRANITE patients tested by ELISPOT
- Association of PFS and peak ex vivo ELISPOT responses was apparent, indicating that ex vivo ELISPOT may be a surrogate for PFS
- GRANITE demonstrated a favourable safety and tolerability profile
- No patients discontinued study treatment due to an adverse event (AE)
- Common AEs were the mild systemic and local effects associated with any potent vaccine
- One treatment-related serious AE (fatigue) occurred in the GRANITE arm but patient continued GRANITE treatment without recurrence upon recovery
Gritstone recognises a need for continued follow-up to “fully assess” the effects of GRANITE and determine whether a plateau of improved PFS, which indicates durable clinical benefit, is achieved. Gritstone bio’s co-founder, President, and CEO Dr Andrew Allen is “excited by the potential” seen in GRANITE to extend both progression-free and overall survival “in a disease where relentless progression is the rule with existing therapies”.
“The field of neoantigen-targeting immunotherapy is evolving rapidly, and the focus is shifting to patients with lower volume disease. Notably, patients with newly diagnosed metastatic disease who have lower ctDNA at study entry and thereby relatively low disease burden, could benefit from this type of immunotherapy.”
More time needed
Dr Allen commented that “typically”, success for immunotherapy “manifests as an elevated plateau in PFS and overall survival Kaplan-Meier curves, and we may be seeing this in our low disease burden population.”
“We need more time to let these data mature.”
The “low and stable” ctDNA measurements in “most” GRANITE patients are “encouraging”, says Dr Allen, as that pattern is “not typically seen in patients about to develop disease progression”. There is also “opportunity for greater effects in tumours more typically amenable to immunotherapy” in the potential benefit observed in MSS-CRC, a “notoriously ‘cold’ tumour”.
“These data support further exploration of GRANITE in frontline MSS-CRC and in other low burden (neo)adjuvant settings. With this new dataset in hand, we continue to actively explore several strategic and funding alternatives to rapidly advance our innovative immunotherapy for the benefit of patients.”
Head above water
The company statement also confirmed that Gritstone has engaged a financial advisor to support its exploration and review of potential “value-maximising strategies”. While Gritstone “does not intend to discuss or disclose further developments”, speculation continues.
Evercore ISI analyst Jonathan Miller is quoted by Fierce Biotech wondering if the company’s cash runway is “functionally no later than” the end of the year. Although “on the face of it” the progress is positive, the data have “limitations”, such as a shift away from patients with more aggressive disease. Miller believes that if Gritstone can keep tracking patients, the extend follow up can continue to look encouraging, but questions the company’s future.
“They don’t have flexibility to run this data out much further, add [patients], or explore [the] adjuvant setting.”
We look forward to welcoming Gritstone’s EVP and Head of R&D, Dr Karin Jooss, to the Congress in Barcelona this month, to share insights in the Cancer and Therapeutic Vaccines track. Get your tickets to join us here, and don’t forget to subscribe to our weekly newsletters for the latest vaccine news.

by Charlotte Kilpatrick | Oct 1, 2024 | Therapeutic |
In an article for npj vaccines in October 2024, researchers present their investigation into the efficacy of a combination of DNA vaccine encoding mouse GPRC5D and PD-1 in preventing and treating multiple myeloma (MM). MM “remains largely incurable”, but the GPRC5D, “highly expressed” in MM, presents a “compelling” immunotherapy candidate. The research suggests that GPRC5D-targeted DNA vaccines are “versatile platforms” for treating and preventing MM.
Managing MM
Multiple myeloma (MM) is the second most prevalent haematological malignancy, characterised by the accumulation of malignant plasma cells in bone marrow. Most MM cases are preceded by monoclonal gammopathy of undetermined significance (MGUS), which can reduce a person’s life expectancy by “more than 4 years”. Around 3.5 million people are affected by MGUS in the United States. Smouldering MM (SMM), distinguished from MGUS for clinical reasons, is an asymptomatic clonal plasma cell disorder between MGUS and MM.
MM treatment has been “transformed with the advent of antibody-based therapies”, with chimeric antigen receptor (CAR) T-cell therapies that target the B-cell maturation antigen (BCMA) showing “considerable promise”. However, the pattern of BCMA expression is heterogeneous, responsible for “varied treatment responses” and the surface expression can “fluctuate” because of gamma secretase-mediated shedding of the extracellular domain. Furthermore, antigen escape has been noted in patients with MM who experienced relapse after BCMA-targeted CAR T-cell therapy.
“Exploring immunotherapies targeting alternative antigens may help counteract antigen escape and provide effective treatment options for patients who relapse after BCMA-targeted CAR T-cell treatment.”
A new vaccine target
C protein-coupled receptors (GPCRs) are the “largest and most diverse” group fo membrane receptors in eukaryotes; humans have almost 1000 different GPCRs. GPCRs are classified into six classes (A-F), among which class C GPCRs initiate metabolic steps to modulate cellular activity.
Orphan GPCR class C group 5 member D (GPRC5D) is expressed in the hair follicle and the bone marrow of patients with MM, as well as in MGUS and SMM. The GPRC5D mRNA is overexpressed between two and four times in MM plasma cells compared to normal plasma cells, and immediate expression is seen in MGUS and SMM.
“GPRC5D is an emerging novel immunotherapeutic and preventive target for MM.”
Although DNA vaccines are a “promising” alternative to mRNA vaccines, with “lower cost and better stability”, they have not yet been widely adopted in clinical practice. DNA cancer vaccine development faces “significant challenges” such as nonspecific formulations, thermal instability, toxicity, and ineffectiveness. However, the authors believe that recent advancements have “greatly enhanced” the clinical efficacy of DNA vaccines in cancer treatment.
The study
In their research, the authors attempted to develop DNA vaccines against MM using plasmids expressing GPRC5D. First, they evaluated a mouse GPRC5D DNA vaccine in the 5TGM1 murine myeloma model, which “closely mimics” human MM. Cancer prevention activity was examined through administration of the DNA vaccine before tumour cell inoculation. The mice that received the mGPRC5D vaccine developed “significantly smaller” tumours than the control mice, and all animals in the mGPRC5D group were alive at day 33.
With ELISA, the authors evaluated the humoral response by measuring the levels of mGPRC5D-specific antibody in the serum collected 5 days after boost. They found a “marked increase” in serum IgG levels in the mGPRC5D group. To explore the possible mechanisms of the antitumour effect of the vaccine, they analysed immune cells in the spleen and tumours through flow cytometry. The percentage of various immune cell populations “significantly increased” in the mGPRC5D-immunised mice.
The research also considered the therapeutic efficacy of the mGPRC5D vaccine in combination with PD1 Ab treatment. After tumour inoculation, mice received two injections of 20µg mGPRC5D vaccine or the control plasmid at 2-week intervals, along with intraperitoneal administration of anti-PD1 antibody. Mice that received either the vaccine or anti-PD1 Ab showed a “moderate inhibitory effect”, but those treated with the combination exhibited “significant inhibition of tumour development”.
When comparing tumour weights in mice, the authors found “significantly” lower weights in the mGPRC5D and PD1 Ab group than in the control group or each monotherapy group. They also assessed the ability of the vaccine to induce TNFα or IFNγ responses in mouse splenocytes with the ELISPOT assay. Splenocytes from mice that received either mGPRC5D or PD1 Ab exhibited a “significant” increase in the number of spots, and a further increase was observed in the group that had the combination. The combination group had higher frequencies of TNFα+CD8+, IFNγ+CD8+, TNFα +CD4+, and IFNγ+CD4+ T cells in the spleen.
In a flow cytometric analysis of immune cell populations in the spleen, the authors found that treatment with mGPRC5D increased the frequency of CD4+ T cells by over 150% and CD8+ T cells by over 30%. PD1 Ab treatment increased the frequency of both cells by more than 100%. The combination had a “more pronounced effect”; CD4+ T cells increased more than 350% and CD8+ T cells increased by more than 130%. Similar observations were made for DCs, Mϕ, and NK cells in the spleen. For tumour-infiltrating lymphocytes (TILs), the combination approach increased the population of CD8+ and CD4+ T cells, DCs, Mϕ, and NK cells more than the monotherapies.
A human vaccine
As the peptide sequences of mGPRC5D and hGPRC5D are only ~81% identical, a human version of the vaccine is needed. The researchers developed a nanoplasmid construct expressing human GPRC5D (Nano-hGPRC5D). Prophylactic studies found that tumour growth was “significantly suppressed” in the mice group that received Nano-hGPRC5D, which also presented a “marked increase” in serum IgG levels. Other findings include a “significant increase” in the levels of cytokines in the Nano-hGPRC5D group, which suggests a “robust activation of inflammatory cytokines” upon vaccination.
In the spleen and tumours of hGPRC5D-immunised mice, percentages of CD3+, CD4+, and CD8+ T cells and DCs were “significantly increased”. Furthermore, higher frequencies of Th1 secretory cytokine-positive CD3+ T cells were observed in this group. A long-acting protective effect against tumours was implied in “significantly higher percentages” of effector and central memory T cells in the splenocytes of the hGPRC5D group. CD8+ T cells stimulated with the hGPRC5D peptide pool exhibited “superior proliferative ability” compared to the control.
Therapeutic combination
To evaluate the therapeutic efficacy of Nano-hGPRC5D in combination with PD1 Ab, the authors used syngeneic murine models. The combination resulted in “significant tumour regression” compared to either treatment alone. Levels of TNFα, IFNγ, IL-6, IL-12p40, and IL-12p70 increased “significantly” in the combination group, and ELISpot analysis revealed more TNFα- or IFNγ-positive cells in the combination group.
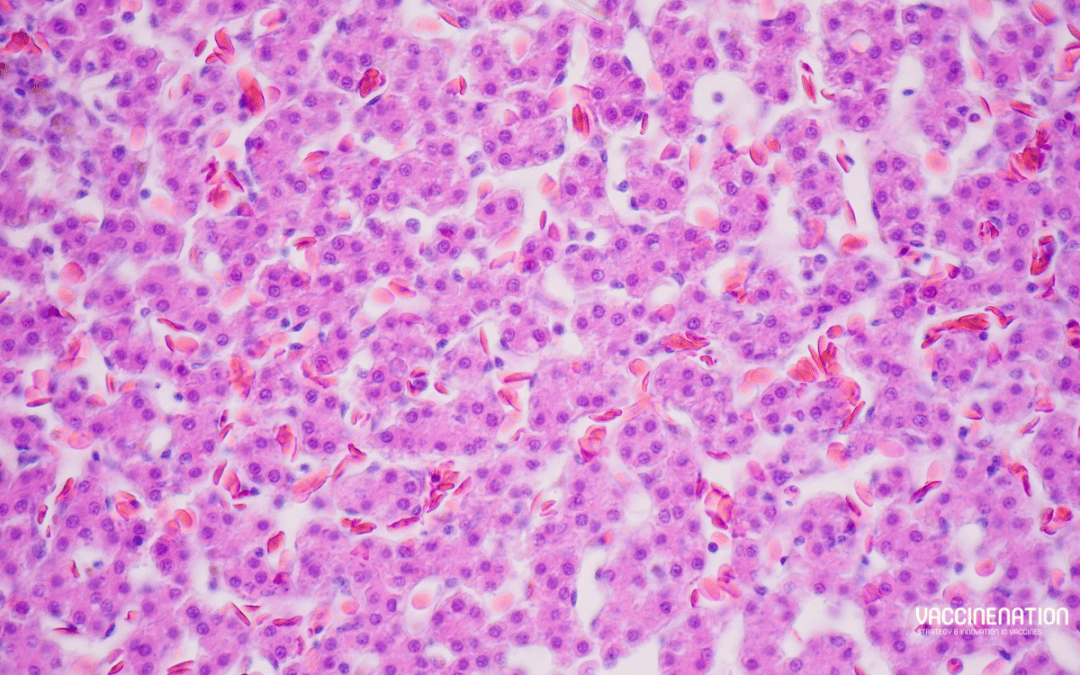
In a flow cytometric analysis of immune cell populations in the spleen and tumour, the combination caused an increase in effector CD8+ and CD4+ T cells, DCs, Mϕ, and NK cells, but a decrease in Treg cells. H&E staining of tumour sections revealed necrotic lesions in the hGPRC5D and combination groups, but the lack of gross histological damage in several major organs supports the safety and clinical potential of the vaccine or combination.
Analysis of the immune cells revealed a “marked increase” in CD3+, CD8+, and CD4+ T cells in the splenic marginal zones of the combination group, consistent with flow cytometry data. There was also an increase in B lymphocytes and follicular DCs in this group. For TILs, the combination therapy also increased the number of CD8+ and CD4+ T cells.
Improving outcomes
Despite therapeutic advancements, high-risk patients with MM “continue to have poor outcomes”, and there are limited agents to prevent MM or progression from MGUS and SMM. The results from the study suggest that PD1 blockade “enhances tumour growth inhibition” in mice treated with the DNA vaccine and highlight the potential of the DNA-based GPRC5D vaccine to “overcome self-tolerance and the prospects of advancing” into clinical trials.
For the latest on cancer vaccine development and combination approaches to disease control, join us at the Congress in Barcelona next week. Don’t forget to subscribe to our weekly newsletters for more vaccine updates.

by Charlotte Kilpatrick | Sep 25, 2024 | Therapeutic |
Anixa Biosciences announced a strategic plan for a Phase II study of its breast cancer vaccine in September 2024. The proposed trial follows a Phase I trial at Cleveland Clinic with grant funding from the United States Department of Defence. The trial will evaluate the efficacy of the vaccine administered in combination with chemotherapy and Keytruda in the neoadjuvant setting. This means that it can enrol a broader range of patients across multiple types of breast cancer.
A unique target
Researchers at Cleveland Clinic identified a protein called alpha-lactalbumin, present only in healthy breast tissue engaged in lactating; it becomes “retired” when the person stops nursing their child and does not exist in any other cell in the body. However, it does appear in “many types” of breast cancer, including the “aggressive and deadly” Triple Negative Breast Cancer (TNBC). By developing vaccines that target alpha-lactalbumin, Anixa hopes that the immune system can destroy cancer cells and prevent tumours from forming.
Moving forward
The Phase I clinical trial in the breast cancer vaccine has produced “positive” clinical data, so a cancer vaccine discovery programme has commenced in collaboration with Cleveland Clinic. This will explore additional cancer vaccine opportunities for “intractable” cancers such as high incidence malignancies in lung, colon, and prostate.
The Phase II trial will evaluate the efficacy of a combination of the vaccine, chemotherapy, and Keytruda in a neoadjuvant setting, seeking to reduce tumour burden and prevent recurrence, with “intent to improve survival”. Trial objectives include evaluating the immunological response to the vaccine and comparing clinical efficacy of standard of care therapy alone with the vaccine plus standard of care therapy. It is expected to begin in 2025 and will last between two and three years.
The trial will enable Anixa to engage more patients with various types of breast cancer. This has potential to address the increasing therapeutic market for breast cancer as prevalence and screening increases drive demand for treatment. The development path for breast cancer treatment is expected to be shorter than primary prevention.
Accelerated treatment
Dr Amit Kumar, Chair and CEO of Anixa Biosciences is excited to unveil the plan, “bringing us one step closer to a potentially transformative therapy for breast cancer patients”.
“By targeting treatment rather than prevention, we can reach a broader patient population and potentially expedite the process of regulatory approval and partnerships. This trial marks a key milestone in advancing our mission to fight cancer through innovative therapies.”
As the Phase II trial will focus on the therapeutic market, data will be used for other studies for “both recurrence prevention and primary prevention with partners in the future”.
Join us at the Congress in Barcelona next month for more on cancer treatment strategies and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Sep 19, 2024 | Therapeutic |
In September 2024, Brenus Pharma announced the completion of a $25 million Series A financing round and receipt of non-dilutive funding to take the STC-1010 cancer vaccine through proof-of-concept in first-line settings for metastatic colorectal cancer patients. STC-1010 is the first candidate based on Brenus Pharma’s STC (Stimulated Tumour (ghost) Cells) technology platform, which offers a new type of precision treatment for a “significant public health challenge”. The platform will be deployed in humans from the end of the year, beginning with STC-1010.
STC platform
Brenus Pharma’s STC platform is designed to educate the immune system to “recognise and anticipate escape mechanisms” in cold tumours. Four key stages happen after injection:
- APC (antigen-presenting cell) cross-priming activation
- TILs (tumour-infiltrating lymphocytes) pool generation
- TILs expansion
- Tumour cell destruction
The technology “not only treats the immediate threat, but also defends the immune system against tumours that may appear later”, reducing a risk of relapse. This is achieved through the education of a patient’s immune system through the “widest panel of therapeutic targets currently available”.
Trials
STC-1010 will be administered as a first-line treatment in patients with unresectable metastatic colorectal cancer (mCRC) resistant to immunotherapies. It will also be tested in other types of gastric tumours, including those of the pancreas and liver. The second candidate in development, STC-1020, will be developed in other solid tumour indications. The team is optimistic that the platform products can become a “permanent part of precision medicine”.
The Phase I/IIA study of STC-1010 is known as “BreAK-CRC”; it is under review by the European regulatory authorities in preparation for participation of clinicians in early-phase immuno-oncology units in Europe and the United States. Phase I will evaluate the tolerability of different dose levels, combined with low dose immunostimulants and standard chemotherapy. The Phase IIA study will evaluate treatment efficacy, with a focus on progression-free survival at 12 months.
Achieving ambitious goals
Jacques Gardette, Chair of BIOJAG, confirmed that “Brenus Pharma now has our full attention to help the company achieve its ambitious goals” as it takes a “major step forward”.
“The arrival of investment professionals in our young company confirms the interest we are arousing…I’m convinced that the constant commitment and innovation of the Brenus team have built a solid foundation for tackling one of the world’s most complex therapeutic challenges.”
Mr Gardette commented on the “boldness, achievement, and resilience” demonstrated by Brenus in its “rapid development”. Dr Paul Bravetti, CEO of Brenus Pharma, reflected that the investment interest is an “important milestone” that confirms the platform’s potential.
“I would like to thank all our team for their motivation and their passionate work to rapidly bring a new therapeutic solution to patients. Our shared ambition is to position our platform at the forefront of the national and international scene, and to become a leader in next-generation cancer immunotherapies.”
Marie Chambodut, Partner and Investment Director at Angelor, is “proud” to lead the strategic transaction.
“We look forward to joining Paul and his exceptional team in transforming Brenus into a global player in precision immuno-oncology, bringing solutions to millions of patients experiencing treatment failure, and contributing to the development of the French biotherapeutics industry.”
Investment Manager at Noshaq, Hélène Sabatal, is “delighted” to support the development of the “cutting-edge technological platform”.
“We are convinced of its future impact for patients currently without concrete therapeutic solutions.”
For the latest in cancer vaccine development and technology, join us at the Congress in Barcelona next month, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Sep 16, 2024 | Therapeutic |
In September 2024, IO Biotech announced “promising” data from its Phase II basket trial of IO102-IO103 in combination with Merck’s anti-PD-1 therapy KEYTRUDA (pembrolizumab). These results were shared in a conference presentation that included clinical and biomarker data from patients with recurrent or metastatic (advanced) squamous cell carcinoma of the head and neck (SCCHN) with PD-L1 CPS ≥ 20. The study met its primary endpoint and identified a safety profile consistent with prior studies.
IO102-IO103
IO Biotech’s lead product candidate is IO102-IO103, which combines two wholly owned T-win vaccines designed to “activate and expand” T cells specific for IDO and PD-L1. T-win is an immune-modulating vaccine technology that is directed against tumour cells and the “most important” immune-suppressive cells in the tumour microenvironment (TME). Many types of solid tumours and immune-suppressive cells (Tregs and TAms) in the TME overexpress IDO and/or PD-L1. Thus, the combination of the two vaccines is intended to “have a synergistic effect” that leads to “enhanced cell killing”.
The Phase II basket study is a non-comparative, open-label trial that investigates the safety and efficacy of a combination of IO101-IO103 with pembrolizumab as a first-line treatment in up to 60 patients with metastatic non-small cell lung cancer (NSCLC) with PD-L1 TPS ≥ 50% and recurrent or metastatic SCCHN with PD-L1 CPS ≥ 20. The primary endpoint is overall response rate (ORR).
Promising data
Data from 18 efficacy evaluable patients revealed:
- The achievement of the primary endpoint – confirmed 44.4% overall response rate (ORR) in a PD-L1 high population of patients with SCCHN irrespective of HPV status.
- An “encouraging” 6.6-month median progression-free survival (PFS).
- A 66.7% disease control rate (DCR).
- A safety profile that is consistent with previously reported data from a combination approach.
- The detection of T-cell responses to both IO102 (targeting IDO) and IO103 (targeting PD-L1) after treatment.
Dr Jonathan Riess, principal investigator of the trial and Director, Thoracic Oncology at UC Davis Comprehensive Cancer Centre, is encouraged by the data in support of the combination approach.
“Given the need for new treatment options that are effective, safe, and accessible for head and neck cancer patients, further investigation of this combination should be conducted to build on the findings of this Phase II trial.”
Chief Medical Officer of IO Biotech, Dr Qasim Ahmad described “accumulating” evidence that the combination could be a “safe and efficacious first-line treatment for patients with a range of cancers”. This includes those with metastatic and “difficult-to-treat disease”.
“Importantly, with mPFS of 6.6 months, more than half of the patients in this trial had over 180 days of progression-free survival. These data are supportive of further investigation of this combination regimen as part of our commitment to transform the lives of cancer patients through our novel therapeutic vaccine.”
For more cancer vaccine updates at the Congress in Barcelona next month, get your tickets to join us here, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Sep 13, 2024 | Therapeutic |
King’s College London shared in September 2024 that an mRNA cancer immunotherapy (mRNA-4359), targeted for patients with lung cancer, melanoma, and other solid tumours, has shown promise in a Phase I trial. The first-in-human study of the therapy involved 19 patients with advanced stage cancers and found that the immunotherapy prompted an immune response against cancer and was well tolerated. Although this was a small study, the researchers are encouraged that their results support further investigations.
Potential in trial
The Phase I trial was designed to test the safety and tolerability of the immunotherapy, with secondary and tertiary objectives exploring the radiographic and immunological responses. 8 out of 16 patients whose responses could be evaluated demonstrated that tumour size did not increase, and no new tumours appeared.
The immunotherapy also activated the immune system in patients, generating immune cells that could recognise two proteins of interest: PD-L1 and IDO1. In some patients the immunotherapy increased levels of “important immune cells that can kill cancer cells” and reduced levels of other immune cells that inhibit the immune system’s response. The researchers acknowledge that their study was small and focussed on safety and finding an optimal dose. However, they continue to recruit patients with melanoma and lung cancer.
An important first step
UK Chief Investigator of the trial is Dr Debashis Sarker, Clinical Reader in Experimental Oncology in the School of Cancer and Pharmaceutical Sciences and consultant in medical oncology at Guy’s and St Thomas’ NHS Foundation Trust. Dr Sarker described the study as in “important first step in hopefully developing a new treatment for patients with advanced cancers”.
“We have shown that the therapy is well tolerated without serious side effects and can stimulate the body’s immune system in a way that could help to treat cancer more effectively. However, as this study has only involved a small number of patients to date, it’s too early to say how effective this could be for people with advanced stage cancer.”
The trial is continuing recruitment of patients in a “huge international effort” across the UK, USA, Spain, and Australia. Dr Kyle Holen, Senior Vice President and Head of Development, Therapeutics and Oncology, Moderna, is “encouraged” by the results. They demonstrate “potential to elicit strong antigen-specific T-cell responses while maintaining a manageable safety profile”.
“This novel approach could be a key component in shifting the tumour microenvironment towards a more immune-permissive state, offering potential hope for patients with advanced solid tumours.”
Professor Tariq Enver, Director of the Cancer Research UK City of London Centre, congratulated the team for “taking us a step closer to personalised cancer vaccines”.
“Through his role supporting training at our centre, Debashis continues to inspire the next generation of clinician scientists to drive life-saving breakthroughs in biological cancer therapies.”
For more insights into cancer vaccine development at the Congress in Barcelona, get your tickets here, and don’t forget to subscribe to our weekly newsletters for the latest news.

by Charlotte Kilpatrick | Sep 12, 2024 | Therapeutic |
Researchers at the University of Birmingham announced the launch of a trial to study the use of an mRNA cancer vaccine in the treatment of pancreatic cancer in September 2024. In collaboration with the University Hospitals Birmingham NHS Foundation Trust (UHB), the researchers aim to recruit patients who are undergoing surgery to remove pancreatic ductal adenocarcinoma (PDAC). These patients will either receive the investigational cancer vaccine in combination with chemotherapy or chemotherapy alone.
Pancreatic cancer
Pancreatic cancer is “among the deadliest cancer globally”, with a survival rate over 10 years of just 5% in England. Physical symptoms often appear only when the cancer has developed to an advanced stage, limiting treatment opportunities. Pancreatic ductal adenocarcinoma (PDAC) is an “extremely aggressive” that accounts for 90% of all pancreatic cancers.
Dr Shivan Sivakumar, Principal Investigator of the trial, Associate Professor in Oncology at the University of Birmingham, and Consultant Medical Oncologist at Queen Elizabeth Hospital Birmingham (QEHB), is “more familiar than most with the devastating nature of this disease”, which is the 5th biggest cancer killer in the UK.
“Sadly, pancreatic cancer is typically diagnosed at a late stage, when curative surgery is no longer an option. The problem is exacerbated by the fact that for the ‘lucky’ 1 in 10 who are eligible for surgery, the recurrence rate of pancreatic cancer after surgical treatment is over 80%.”
A new hope
The investigational therapeutic cancer vaccine deploys mRNA to deliver “instructions” for neoantigens found in a patient’s cancer. Samples of each patient’s tumour tissue and blood are sent to laboratories after surgery for vaccine design and manufacture. This approach of “training the immune system to recognise and attack cancer cells” could potentially prevent cancer recurrence and increase the possibility of curing the patient.
Dr Sivakumar is “incredibly proud” that the Queen Elizabeth Hospital Birmingham is the first site in Europe to enrol a patient in the trial.
“This achievement highlights Birmingham’s leading role in advancing cancer treatment, offering new hope for patients battling one of the most challenging cancers we face today.”
Professor Kiran Patel, Chief Medical Officer at University Hospitals Birmingham NHS Foundation Trust commented that “we are very fortunate to have exceptional infrastructure and world-class talent that positions us perfectly to lead in vital areas of cancer research”.
“This trial showcases the expertise and dedication of our medical professionals, and the fantastic teams supporting them, who are at the leading edge of clinical research here in Birmingham. To be the first site to open in Europe reaffirms our role as a national and international centre for cutting-edge oncology and highlights our commitment to improving patient outcomes through pioneering approaches.”
Head of Research and Development Operations at UHB Jo Gray recognised the role of the National Institute for Health and Care Research (NIHR) Wellcome Trust Clinical Research Facility (CRF) in providing “expert care to patients receiving experimental therapies”.
“Birmingham is the first site outside of North America to open and to enrol a patient onto this complex, early phase trial that addresses an important need to identify better post-surgery treatments for pancreatic cancer.”
Professor Neil Hanley, Head of the College of Medical and Dental Sciences at the University of Birmingham stated that the research “epitomises why the University of Birmingham and its tremendous partnership with UHB is delivering life-changing impacts”. Professor Hanley hopes to “tilt” the discoveries of the pandemic towards a “much-needed world of new cancer treatments”.
“Birmingham is the ideal place to open this trial, with one of the leading pancreatic cancer units in the UK and serving a super diverse population.”
Head of Research at Pancreatic Cancer UK, Dr Chris Macdonald looks forward to “hope on the horizon”.
“We are absolutely delighted that Queen Elizabeth Hospital Birmingham is the first site in Europe to enrol a patient to an individualised pancreatic cancer vaccine trial. We will be following the results with great interest, as the potential here cannot be understated. If this research proves successful, the vaccine could be a vital new weapon against the deadliest common cancer.”
For more on the potential that mRNA might have for cancer therapy, join us in Barcelona for the Congress this October, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Sep 11, 2024 | Therapeutic |
GSK announced in September 2024 that it has completed the primary objective data analysis from the Phase II part of its TH HSV REC-003 trial. The trial is a combined Phase I/II proof-of-concept study to assess the potential clinical efficacy of GSK’s early-stage therapeutic herpes simplex virus (HSV) vaccine candidate, GSK3943104, before it progressed to further clinical development. The results indicate that GSK3943104 did not meet the study’s primary efficacy objective, which means it will not progress to Phase III studies.
GSK3943104 in study
The first-time-in-human (FTiH) study sought to evaluate the reactogenicity, safety, immune response, and efficacy of GSK’s investigational herpes simplex virus (HSV)-targeted immunotherapy. It was conducted in two parts; the first assessed different formulations in healthy participants between the ages of 18 and 40 years. The second part assessed the two formulations in participants between the ages of 18 and 60 with recurrent genital herpes.
Although no safety concern was observed, GSK3943104 did not meet the primary efficacy objective. However, the TH HSV REC-003 study will continue for routine safety monitoring and to generate follow-up data, which could offer valuable insights into recurrent genital herpes.
More innovation needed
GSK commented on the “unmet medical need and burden associated with genital herpes”, calling for “innovation in this area”.
“GSK intends to evaluate the totality of all these data and other studies to progress future research and development of its HSV programme.”
WHO states that around 3.7 billion people under the age of 50 have herpes simplex virus type 1 (HSV-1) infection; this is the “main cause” of oral herpes. An estimated 491 million people between the ages of 15 and 49 have herpes simplex virus type 2 (HSV-2) infection, the “main cause” of genital herpes. Although most HSV infections are “asymptomatic or unrecognised”, infection with HSV-2 “increases the risk of acquiring and transmitting HIV infection”.
For the latest updates on therapeutic and prophylactic vaccine development at the Congress in Barcelona this October, get your tickets to join us here. Don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Sep 11, 2024 | Therapeutic |
In September 2024, OSE Immunotherapeutics announced the launch of an international Phase III clinical trial of its off-the-shelf neoepitope-based therapeutic cancer vaccine, Tedopi. The trial, named ‘Artemia’, will compare the efficacy and safety of Tedopi monotherapy with the standard of care in HLA-A2 positive patients with metastatic non-small cell lung cancer (NSCLC) with secondary resistance to immune checkpoint inhibitor (ICI). The primary endpoint is overall survival.
Tedopi and the Artemia trial
NSCLC accounts for 85% of all lung cancers, and the HLA-A2 phenotype represents around 45% of the population. The target population for Tedopi in second line is “considered as rare with high unmet medical needs”. This could be up to 46,000 patients a year across “seven major markets”.
Tedopi is a novel T-cell epitope-based cancer vaccine that targets five tumour-associated antigens. It is an activating and differentiated off-the-shelf immunotherapy expanding tumour specific T-lymphocytes in HLA-A2 cancer patients. It is being investigated in several Phase II trials as well as Artemia, a confirmatory Phase III clinical trial. This is intended to support the registration of Tedopi in second-line treatment of NSCLC in Europe and North America, alongside the companion diagnostic test for HLA-A2 positive patients.
Artemia is an international, randomised, open-label Phase III trial in the United States, Canada, Europe, and the United Kingdom. It is expected to include 363 patients.
Extending survival
Dr Silvia Comis, Head of Clinical Development and Regulatory Affairs at OSE Immunotherapeutics is “very pleased” that the last registration development step of the vaccine has started, supported by “positive and promising results” from the first Phase III in third-line treatment in NSCLC.
“These results demonstrated that re-arming the immune system with vaccine in metastatic patients can extend survival and preserve quality of life in the targeted population.”
Dr Nicolas Poirier, OSE Immunotherapeutics’ Chief Executive Officer looks forward to “confirming the therapeutic benefit of Tedopi for metastatic cancer patients”.
“Tedopi is the most advanced therapeutic cancer vaccine in clinical development and the first treatment option to address the high unmet medical need and large untapped market in advanced and metastatic second-line NSCLC.”
Dr Stephen Liu, associate professor and director of Thoracic Oncology at Georgetown University Lombardi Comprehensive Cancer Centre, is coordinating investigator for the United States and Steering Committee member. Dr Liu is “excited to see the Artemia trial activated in the US”.
“With an off-the shelf vaccine approach, we can offer a safer and more tolerable approach than chemotherapy for patients with advanced lung cancer. By properly engaging a patient’s own immune system, we hope to significantly extend survival.”
For more insights into cancer vaccine development and research, join us at the Congress in Barcelona this October, and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Sep 10, 2024 | Therapeutic |
In September 2024, Evaxion Biotech announced positive topline data from a Phase II trial of EVX-01. This is part of a one-year interim analysis of the trial assessing EVX-01 in combination with MSD’s anti-PD-1 therapy, KEYTRUDA, in patients with advanced melanoma. These data show that 11 out of 16 patients had objective clinical responses and 15 out of 16 patients had a reduction in tumours (target lesions). Complete data will be presented at a conference in September 2024.
EVX-01 in trial
EVX-01 is Evaxion’s lead clinical asset, a personalised peptide-based cancer vaccine intended for first-line treatment of multiple advanced solid cancers. The personalised therapy is designed with Evaxion’s AI-Immunology platform and is tailored to target each patient’s unique tumour profile and immune characteristics.
The Phase II study is a self-sponsored open-label, single-arm, multi-centre trial to evaluate the efficacy and safety of EVX-01 vaccination in combination with MSD’s KEYTRUDA in treatment-naïve patients with metastatic or unresectable malignant stage III or IV melanoma. It is being carried out in collaboration with teams from Italy and Australia.
Evaxion reports that these topline data reveal a 96% Overall Response Rate (ORR) with 11 of 16 patients having objective clinical responses and 15 of 16 patients having reduction of their tumours. CEO of Evaxion, Christian Kanstrup, is “very excited” about the data, which “strongly support both the clinical profile of EVX-01 as a promising personalised cancer treatment” and the “unique predictive capabilities” of AI-Immunology.
“To present Phase II efficacy data for an AI-designed vaccine is a major milestone for Evaxion. Huge unmet medical needs remain in the field of melanoma, and we believe that EVX-01 could potentially be an improved treatment option for patients.”
We look forward to hearing from senior representatives of Evaxion at the Congress in Barcelona this October, so do get your tickets to participate in their sessions, and don’t forget to subscribe to our weekly newsletters for more vaccine updates.

by Charlotte Kilpatrick | Sep 3, 2024 | Therapeutic |
A paper in Science Advances in August 2024 describes XPO1 (Exportin-1/CRM1) as a “bona fide tumour antigen” recognised by natural killer (NK) cells. With implications for vaccine development, the research identifies an opportunity for a personalised approach to NK cell therapy for solid tumours. The authors, led by a team at the University of Southampton, believe that “hijacking” the protein is a viable avenue of investigation.
Natural killer cells
The paper states that natural killer (NK) cells are becoming “increasingly recognised for their anticancer activity”. Their functions are “tightly controlled by a diverse repertoire of cell surface receptors”. Killer cell immunoglobin-like receptors (KIRs) are an “important family” of NK cells receptors, forming a polymorphic family of receptors with human leukocyte antigen (HLA) class I ligands. KIRs are “implicated in susceptibility to, and the outcome of”, a range of cancers, and contribute to heterogeneity within the innate immune response to malignancy.
KIRs can be activating or inhibitory; although the HLA class I ligand specificities of the inhibitory KIR are “relatively well defined”, the ligand specificities of the activating KIR are “much harder to identify”. However, recent research suggests that activating KIR can have an HLA class I-restricted peptide specificity. KIRs recognise families of peptide:HLA complexes in a motif-based manner, which allows recognition of different combinations of peptide and HLA.
Activating KIRs have been linked to protective responses to several cancers, including haematological malignancies. There is “potential” for KIR2DS2 binding peptides to be tumour-associated antigens derived from endogenously expressed proteins that are up-regulated during tumorigenesis. In the context of a lack of cancer-associated peptides that bind activating KIR, the authors sought to investigate this in a proof-of-concept study.
The study
XPO1, a nuclear export protein, is “frequently overexpressed” in cancer and serves as a “driver of oncogenesis”. The paper describes a molecular mechanism underlying a KIR2DS2 specific response against cancer, identifying that the combination of XPO1 and NK cells is associated with longer survival in “multiple” cancers. XPO1 is expressed at “low” levels in healthy cells, which the authors infer are too low to generate an activating signal in KIR2DS2-positive NK cells. They propose that the up-regulation of XPO1 found in cancer can “alter the balance” for NK cell activation in favour of activation of KIR2DS2-positive NK cells.
Professor of Hepatology at the University of Southampton, Salim Khakoo, challenges previous assumptions that killer cells attack cancer cells randomly.
“Our findings actually show how our body’s immune system recognises and attacks these cancer cells.”
Killer cells as “emerging” as a form of immunotherapy that “shows huge promise”, says Professor Khakoo.
“They don’t attack health tissue in the way chemotherapy and other immunotherapies do, so are safer and have [fewer] side-effects than traditional forms of cancer treatment.”
The peptide derived from XPO1 appeared to attract natural killer cells to trigger an immune response, leading to “significantly better survival rates” across a “range of cancers”. This included cancers with higher rates of death, such as liver cancer. Professor Ralf Schittenhelm of Monash University hopes that the research offers a new way of activating killer cells to treat disease effectively.
“We hope it could lead to personalised cancer treatment, especially in cases where traditional therapies have failed. The potential to develop targeted therapies that utilise the body’s own immune system is incredibly exciting.”
The team at Southampton will move to vaccine development in pursuit of the “first vaccine that uses natural killer cells to fight cancer”.
For the latest cancer vaccine development updates at the Congress in Barcelona this October get your tickets here, and don’t forget to subscribe to our weekly newsletters for more.

by Charlotte Kilpatrick | Aug 30, 2024 | Therapeutic |
Research in Nature communications in August 2024 reports a non-human primate model of metabolic post-acute sequelae of SARS-CoV-2 to identify a dysregulated blood chemokine signature in acute COVID-19 that correlates with “elevated and persistent hyperglycaemia” four months post-infection. The authors also report a favourable glycaemic effect of the mRNA vaccine, administered on day 4 post-infection. This approach could help to address “one of the most concerning issues” of long-term health conditions after COVID-19 infection; hyperglycaemia can lead to health complications like diabetes and heart disease.
PASC or Long-COVID
The paper states that between 10% and 30% of people infected with SARS-CoV-2 develop long-term health complications, known as post-acute sequelae of SARS-CoV-2 (PASC) or Long-COVID. These complications fall along a “broad spectrum” from metabolic diseases to conditions with “less obvious metabolic undertones”. Evidence suggests a hyperinflammatory response is “critical” to the severity of acute COVID-19 and the development of metabolic PASC such as hyperglycaemia.
Although it is suggested that the balance between virus survival and effective host responses is based on the metabolic reprogramming of nutrients, the extent to which early disruptions in systemic immune and metabolic homeostasis contribute to metabolic PASC “remains unclear”. Furthermore, a “lack of appropriate animal models” for metabolic PASC means that the mechanisms by which SARS-CoV-2 infection “promotes prolonged hyperglycaemia” are “poorly understood”.
The study
The researchers developed a model using SARS-CoV-2 infected non-human primates (NHPs). African green monkeys (AGMs) were infected intranasally and intratracheally; blood biochemistry, virologic, and immunologic parameters were analysed longitudinally for an 18-week period. Metabolic, virologic, and clinical analyses were also performed on selected tissues at necropsy to “interrogate potential mechanisms that underlie the development” of metabolic PASC.
To explore if vaccination against SARS-CoV-2 during acute infection, prior to multiorgan distribution from the lungs, could elicit a “more favourable” tissue microenvironment that reduces the tissue burden of replication competent SARS-CoV-2 and/or viral fragments, the authors investigated administration of the BNT162b2 vaccine four days after infection. The cohort was split into two groups: unvaccinated (10) and vaccinated (5). The vaccinated group were vaccinated 4 days post infection with the mRNA vaccine BNT162b2.
Findings
The data demonstrate that SARS-CoV-2 infection of AGMs is “associated with early-onset hyperglycaemia”, persisting for at least 18 weeks post infection. However, the vaccination of five of the animals 4 days post infection was associated with a “consistent and significantly lower” blood glucose level over the study period. Dr Clovis Palmer, a lead author of the study, describes the research as a “new frontier in our fight against COVID-19″.
“By showing that the vaccine can have therapeutic benefits even after infection, we can explore new strategies to help those suffering from long-COVID, especially those with symptoms like chronic fatigue that may be linked to metabolic dysfunction.”
Dr Jay Rappaport, co-corresponding author and director of the Tulane National Primate Research Centre commented that the discovery that COVID-19 can “induce diabetes in an animal model” is a “significant advancement in our understanding of the long-term effects”.
“The fact that a COVID vaccine given after infection can have protective effects highlights the importance of innovative research in addressing the ongoing challenges of a pandemic.”
For more on COVID-19 vaccines at the Congress in Barcelona get your tickets here, and don’t forget to subscribe for weekly vaccine updates here.

by Charlotte Kilpatrick | Aug 23, 2024 | Therapeutic |
University College London Hospitals (UCLH) announced in August 2024 that a patient with lung cancer at UCLH is the first to receive a novel cancer vaccine in a clinical trial in the UK. BioNTech’s investigational immunotherapy, BNT166, uses mRNA to present common tumour markers from non-small cell lung cancer (NSCLC) to the patient’s immune system. The vaccine is designed to offer a lower risk of toxicity to health, non-cancerous cells. This study will determine if BNT116 is safe and well tolerated. It is enrolling patients at different stages of NSCLC.
The trial
The trial is intended to establish the safety profile and a safe dose of BNT116 as a monotherapy as well as BNT116 in combination with other treatments for NSCLC to explore if BNT116 has a “synergistic anti-tumour effect” in combination. Around 130 participants will be enrolled in the study at 34 research sites in seven countries; six sites in the UK have been selected.
Consultant medical oncologist Dr Sarah Benafif is leading the study at UCLH and stated that “the strength of the approach” is that the treatment is “aimed at being highly targeted towards cancer cells”.
“In this way we hope that in time we are able to show that the treatment is effective against lung cancer whilst leaving other tissues untouched.”
UCLH Director of Research and Director of the NIHR UCLH Biomedical Research Centre, Professor Karl Peggs emphasised that “developing new approaches to cancer is a major priority for research at UCLH and within the BRC”. Professor Peggs is excited to see the first-in-human research “get started” at UCLH.
“We are able to do this kind of research thanks to our first-rate clinicians and research teams, our track record of working alongside industry, and our facilities and infrastructure which receive crucial support from the NIHR.”
An exciting new era
Professor Siow Ming Lee of UCL reflected that lung cancer “remains the leading cause of cancer deaths worldwide”, causing an estimated 1.8 million deaths in 2020.
“We are now entering this very exciting new era of mRNA-based immunotherapy clinical trials to investigate the treatment of lung cancer, thanks to the foundation laid by the Office for Life Sciences, within the Department for Science, Innovation, and Technology and the Department for Health and Social Care.”
Professor Lee hopes that the research will “provide an opportunity to further improve outcomes for our NSCLC patients, whether in the early or advanced stages”.
Advancing science
The first participant in the trial is Janusz Racz, 67, from London. He decided to participate in the trail “because I hope it will provide a defence against cancer cells” but also because “my participation in this research could help other people in future and help this therapy become more widely available”.
“As a scientist myself, I know that science can only advance if people agree to participate in programmes like this. I work in artificial intelligence, and I am open to trying new things. My family did research about the trial too, and they supported me taking part.”
Science Minister Lord Vallance is pleased to see the vaccine taking its “next important step” with potential to save the lives of “thousands diagnosed with lung cancer every year”.
“With Government support, these trials demonstrate again that the UK’s world-leading life sciences sector is at the forefront of turning research into new treatments like cancer vaccines, which could be transformative for patients up and down the country. We back our researchers so that they can continue to be an integral part of projects that produce groundbreaking therapies, like this one.”
NHS England national cancer director Dame Cally Palmer believes that if this is successful, cancer vaccines could be “revolutionary in vaccinating people against their own cancers to prevent the cancer recurring after their initial treatment”.
“Pioneering work is being undertaken by hospitals throughout the country with their university and industry partners to look at ways of harnessing the body’s own immune system to treat a range of cancers.”
Although a cancer diagnosis is “very worrying”, access to trials and other interventions “provides hope”.
“We expect to see thousands more patients taking part in trials over the next few years.”
For more on cancer vaccine developments, including from representatives of BioNTech, join us at the Congress in Barcelona this October and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Aug 22, 2024 | Therapeutic |
In August 2024 Everest Medicines announced the launch of an Investigator-Initiated Clinical Trial (IIT) assessing the safety, tolerability, immunogenicity, and preliminary efficacy of a personalised mRNA cancer vaccine. EVM16 will be considered as a monotherapy and in combination with PD-1 antibody for patients with advanced or recurrent solid tumours. This is the first-in-human trial for EVM16 and will take place at the Peking University Cancer Hospital and Fudan University Cancer Hospital.
EVM16
EVM16 is a novel personalised therapeutic mRNA cancer vaccine containing neoantigens with “high immunogenicity potential”. These antigens are predicted based on the unique tumour mutations of each patient through Everest’s proprietary neoantigen prediction algorithm. The vaccine “efficiently” delivers neoantigen-encoded mRNA in vivo through a lipid nanoparticle (LNP) delivery system to activate neoantigen-specific tumour-killing T cells and inhibit tumour growth.
Preclinical studies found that vaccination with EVM16 stimulated a “strong” neoantigen-specific T cell response in different mouse models and showed “significant” tumour growth inhibition in the syngeneic B16F10 mouse melanoma model. Preclinical data also revealed a synergistic effect in the combination of EVM16 and a PD-1 antibody, supporting the clinical application of the combination of EVM16 with checkpoint inhibitors. Repeated dosing with EVM16 was “well tolerated and safe” in preclinical toxicity studies. Thus, Everest believes that the vaccine is safe and “has potential to bring benefits to cancer patients”.
An important milestone
Chief Executive Officer of Everest Medicines, Rogers Yongqing Luo, described the initiation of the trial as an “important milestone that demonstrates our commitment to discover and develop a new generation of mRNA immunotherapies for cancer and autoimmune diseases”. The vaccine is the first personalised mRNA cancer vaccine developed “independently” by Everest using the proprietary mRNA platform.
“While establishing leadership positions in nephrology, infectious disease, and autoimmune diseases, Everest will also focus on innovative modalities such as therapeutic mRNA vaccines. We look forward to seeing personalised cancer vaccines become a new clinical treatment method to serve more patients.”
For more on immunotherapy advances at the Congress in Barcelona get your tickets to join us here and don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Aug 15, 2024 | Therapeutic |
In August 2024 CureVac announced the start of the dose-confirmation Part B in its ongoing Phase I study of CVGBM in patients with resected glioblastoma. CVBGM is CureVac’s first investigational cancer vaccine based on the proprietary second-generation mRNA backbone. The vaccine encodes a single fusion protein comprising eight epitopes with “demonstrated immunogenicity” in glioblastoma.
CureVac’s approach
CureVac states that the approach to mRNA-based cancer treatments “enhances antigenic properties of proteins”. A “special transport system” simulates viral infection, which “optimally addresses the immune system”. The therapeutic pipeline comprises “several” mRNA molecules encoding specific tumour-associated antigens. Furthermore, the approach attacks the cancer cells “directly” with RNA and modifies the tumour tissue environment for immune modulation.
The next step
The research involves an open-label study to evaluate the safety and tolerability of CVGBM in patients newly diagnosed and surgically resected MGMT-unmethylated glioblastoma or astrocytoma with a molecular signature of glioblastoma. It is administered as a monotherapy after surgical resection and completion of radiotherapy with or without chemotherapy.
After successful completion of a dose-escalation Part A, the vaccine candidate progresses to dose-expansion in Part B. In Part A 16 patients were involved to test doses between 12µg and 100µg. Safety data has been reviewed and confirmed no dose-limiting toxicities. A 100µg dose is recommended for Part B, which is expected to involve up to 20 patients.
Dr Myriam Mendila, Chief Scientific Officer of CureVac, is pleased with the “successful completion” of Part A.
“The dose expansion part B is important to confirm that we have selected the appropriate dose based on safety and immunogenicity for further studies in patients suffering from glioblastoma.”
Dr Mendila also highlighted the importance of the review by the Data Safety Monitoring Board, which confirmed no dose-limiting toxicities. This “enabled us to move forward to this next part of the study”.
For the latest cancer vaccine developments do make sure you get your tickets to the Congress in Barcelona this October or subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Aug 8, 2024 | Therapeutic |
In August 2024 a paper in Disease Models and Mechanisms presents research that uncovers the earliest cellular mechanisms involved in tumour clearance induced by the Bacillus Calmette-Guérin (BCG) vaccine. Initially developed for use against tuberculosis (TB), the BCG vaccine is the “oldest cancer immunotherapeutic agent in use”. However, little is understood about its initial mechanisms of action. Thus, the authors developed an in vivo assay to visualise the interactions between bladder cancer cells, BCG, and innate immunity in real time and at single-cell resolution.
BCG
BCG has been used as a cancer immunotherapeutic agent for years and is the “most effective treatment to avoid disease relapse” in bladder cancer. Intermediate or high-risk non-muscle-invasive bladder cancer (NMIBC) tumours are treated with intravesical BCG immunotherapy around 2 weeks after transurethral resection. The therapy involves 6 weekly instillations, followed by maintenance therapy of 1 to 3 years. However, this approach has a high rate of adverse effects, the supply chain has worldwide shortages, and some patients are resistant to treatment.
The authors highlight that the mechanisms through which BCG induces anti-tumour activity are “not fully understood” and that BCG therapy has remained “mostly unchanged”. Previous research proposed a multi-step model:
- In steps 1 and 2 BCG binds to and invades the bladder lumen, interacting with the urothelium and tissue-resident macrophages.
- In step 3 BCG is internalised by immune cells and induces an innate immune response that triggers a strong local induction of pro-inflammatory cytokines and chemokines. This stimulates the recruitment of immune cells. Macrophages and other antigen-presenting cells present BCG antigens to T lymphocytes through the major histocompatibility complex class II and trigger an adaptive immune response.
- In step 4 therapy is considered successful if the induction of the adaptive immune response is biased towards Th1 cells. The recruitment of these immune cells leads to the development of granulomatous lesions in the bladder wall.
The zebrafish model
Assessing treatment response in patients is challenging, so animal models of bladder cancer have been used, such as mice. Although mice are considered the “gold-standard xenograft model” for their “highly conserved genetic likeness with humans”, the model has disadvantages. An alternative is the zebrafish; similarities in molecular pathways and drug responses between zebrafish and humans and the “ease in genetic manipulation” allow for “robust” cancer models.
“In zebrafish cancer xenografts, where human tumour cells are injected into zebrafish embryos or adults, cancer features such as proliferation, angiogenesis, metastasis, and interactions in the tumour microenvironment (TME) can be rapidly visualised in real time and at the single-cell level due to the optical transparency of the model.”
Research in zebrafish xenografts “facilitates the rapid identification of novel cancer mechanisms that can be targeted by specific therapeutic approaches”. Additionally, the zebrafish model has supported human tuberculosis research.
The study
The researchers used real-time single-cell-resolution microscopy to demonstrate in vivo in a bladder cancer zebrafish xenograft that BCG immunotherapy “induced cancer cell apoptosis and clearance of tumours through macrophages and TNF signalling”. BCG stimulated a “massive recruitment of macrophages” that were polarised towards a Tnfa-positive pro-inflammatory phenotype.
High-resolution live microscopy revealed that the presence of BCG in the TME induced “profound changes” in macrophage morphology and cell-cell interactions. Without innate immune cells, tumour clearance was “halted”, which demonstrates their importance to BCG’s anti-tumour effects. The authors also demonstrated the utility of their xenografts in a preclinical setting, testing the efficacy of a newly genetically modified BCG vaccine against the conventional BCG vaccine.
Dr Mayra Martínez-López, first author, suggests that BCG immunotherapy is “still rather empirically used”. It is a “very effective immunotherapy” even in comparison with “so many fancy immunotherapies that are being developed”.
“Not only did we unravel the mechanisms involved in the first steps of the vaccine’s anti-tumoral action, we also demonstrated that the zebrafish Avatar model is a powerful preclinical tool for drug discovery in oncology.”
To join discussions about innovative immunotherapies and cancer vaccine strategies, get your tickets to the Congress in Barcelona this October. Don’t forget to subscribe to our weekly newsletters here.

by Charlotte Kilpatrick | Aug 6, 2024 | Therapeutic |
ImmunityBio announced in August 2024 that a clinical trial to study ANKTIVA and the investigational AdHER2DC vaccine in individuals with HER2-expressing endometrial cancer has opened. The trial is sponsored by the US National Cancer Institute (NCI) and seeks to assess the safety and preliminary clinical efficacy of the AdHER2DC vaccine in combination with ANKVITA, pembrolizumab, and lenvatinib before a larger study. Endometrial cancer is the most common gynaecological cancer in the US, affecting more than 65,000 women every year. The 5-year overall survival rate in patients with metastasis is “around 20%”, and treatment options after the second-line treatment are “limited”.
ANKTIVA and AdHER2DC
ANKTIVA is ImmunityBio’s IL-15 superagonist immune enhancer; it was approved by the FDA for BCG-unresponsive non-muscle invasive bladder cancer CIS with or without papillary tumours in April 2024. The AdHER2DC vaccine targets the HER2 protein, which is elevated in 30% of patients with endometrial cancer and in more than 50% of “high-risk subtypes”. The autologous vaccine uses participants’ blood cells that are drawn through apheresis.
The vaccine, a dendritic cell vaccine that is “transduced with an adenoviral vector expressing extracellular domain and transmembrane domain of HER2”, proved to be “well tolerated” and demonstrated “preliminary clinical benefit” in 21 evaluable patients. In this trial, all participants will receive the vaccine and the FDA-approved drugs (pembrolizumab and lenvatinib), and some will receive ANKTIVA.
The study
The Phase I/II study is an open-label, two-arm study; the first phase will determine the recommended dose of each intervention in participants with HER2 positive endometrial cancer. The Phase II section will assess the efficacy of the combination in qualified participants. The study will enrol 60 subjects and is scheduled to complete in 2026. Dr Patrick Soon-Shiong, Executive Chair and Global Scientific and Medical Officer at ImmunityBio, is “pleased to partner with the NCI” on the “important” study.
“We are hopeful that the AdHER2DC investigational vaccine plus ANKTIVA will ‘rescue’ the checkpoint inhibitor pembrolizumab and kinase inhibitor lenvatinib and lead to an improved response compared with the current standard of care in this high-risk population.”
Join us at the Congress in Barcelona this October to hear more on cancer vaccine research and don’t forget to subscribe to our weekly newsletters here.