WHO announced in October 2024 that it is launching the Global Strategic Preparedness, Readiness, and Response Plan (SPRP) to tackle dengue and other Aedes-borne arboviruses. The Plan is intended to reduce the burden of disease, suffering, and deaths from dengue and other Aedes-borne arboviral diseases, like Zika and chikungunya, by “fostering a global coordinated response”. It presents priority actions to control transmission and offers recommendations to affected countries across various sectors. With five “key components”, the Plan is to be implemented over one year until September 2025, demanding US$ 55 million.
“The SPRP is a call to action for all stakeholders – from government agencies and health-care providers to communities and individuals – to join forces in the fight against dengue and other Aedes-borne arboviruses, through innovation, new technologies, and improved vector control strategies.”
Turning the tide
In the foreword by WHO Director-General Dr Tedros Adhanom Ghebreyesus we learn that dengue has “afflicted humanity for centuries, and possibly longer”; the first report of a clinically compatible case is recorded in a Chinese medical encyclopaedia in 992. From a much more contemporary perspective, dengue has spread “rapidly” in the past 20 years, enabled by “increased global travel and the effects of climate change”. Between 2000 and 2019, WHO documented a “tenfold surge” in reported cases, to 5.2 million. Since then, the surge has continued; over 12.3 million cases were reported by the end of August 2024.
The global prevalence and effects of arboviruses like dengue are a “significant threat to public health”, particularly in tropical areas where they are endemic. Addressing this threat demands a “concerted, strategic, and informed response”, which the Director-General hopes to achieve with the SPRP, a “comprehensive plan” to outline ways of controlling Aedes-borne arbovirus transmission in affected countries.
“Our multifaceted approach emphasises integrated surveillance, laboratory diagnosis, vector control, community engagement, clinical management, and research and development.”
This approach should reduce the burden of disease, save lives, and minimise the socioeconomic consequences of these diseases. Furthermore, the Plan includes measures for “safe programming” to ensure interventions are “secure and do not exacerbate the risk” for those who are already vulnerable to disease or those involved in responding to the crisis. Dr Tedros states that prevention and control is a “shared responsibility”.
“Together, we can turn the tide against this disease, protect vulnerable populations, and pave the way for a healthier future.”
Understanding the threat
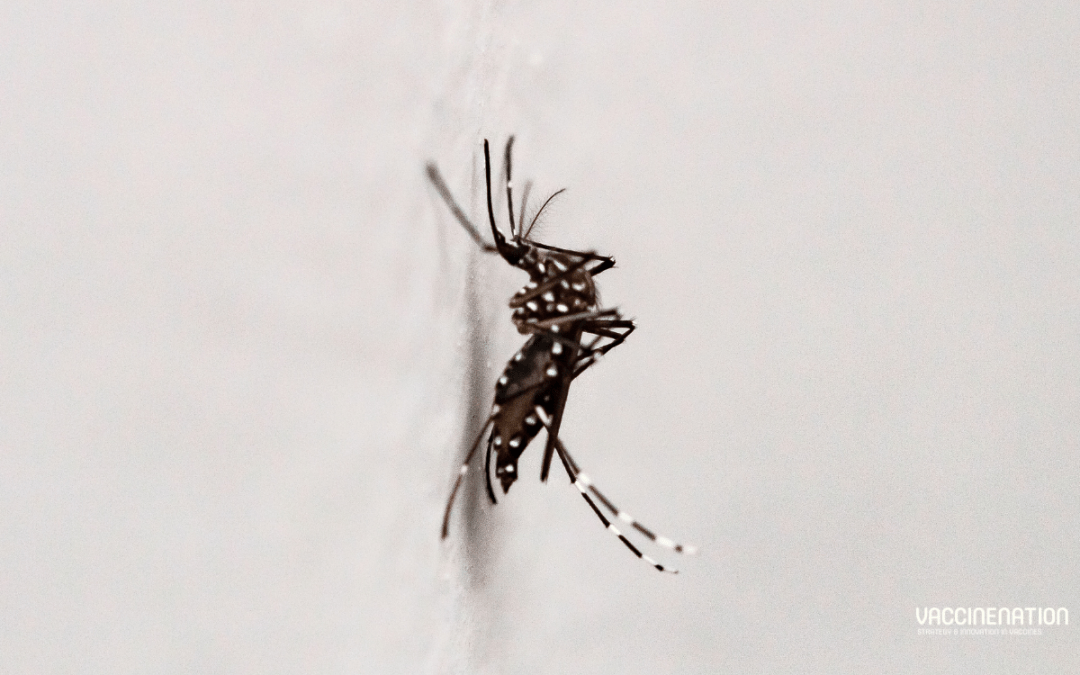
Dengue is a challenge across all of WHO’s regions, endemic in more than 100 countries. Various factors, such as unplanned urbanisation and the effects of climate change, fuel the spread of dengue and other Aedes-borne arboviruses, such as Zika and chikungunya, putting more than four billion people at risk. The growing threat must be addressed with a “robust and dynamic strategy” that accounts for the current global epidemiological landscape. This is complicated by the “still developing” global surveillance system.
Transmission drivers like the effects of climate change and population growth can explain the increase of these infections in some areas, but they also point to the need for a multisectoral approach to prevent and respond to outbreaks.
The Plan
The Plan is intended to “reduce the burden of disease and deaths from dengue and other Aedes-borne arbovirus diseases in all affected WHO regions”. The strategic objective is “to accelerate progress in preventing and controlling dengue and other Aedes-borne arboviral disease outbreaks worldwide”, with the following specific objectives:
- Strengthen global multisectoral coordination and collaboration among stakeholders and partners in preparedness, response, and resilience to dengue and other Aedes-borne arbovirus diseases
- Enhance the capacity of Member States in early detection, reporting, confirmation, and response to outbreaks of dengue and other Aedes-borne arboviruses
- Strengthen the capacity of Member States to implement effective vaccination and integrated vector management strategies for mitigating the transmission of dengue and other Aedes-borne arboviruses
The SPRP combines strategic interventions tailored to local contexts and leverages inter-stakeholder synergies to “confront the challenges” posed by these diseases and move closer to controlling them. The following “interconnected pillars” are included in the multidisciplinary approach:
- Leadership, coordination, planning, monitoring, and prevention of sexual misconduct
- Risk communication and community engagement (RCCE) and infodemic management
- Surveillance, case investigation, and contact tracing
- Travel, trade, and points of entry surveillance and control
- Laboratory and diagnostics
- Integrated vector management and WASH & IPC
- Clinical management and therapeutics
- Operational support and logistics
- Essential health services and systems
- Vaccination
- Research, innovation, and evidence
The 5Cs
The SPRP aligns with WHO’s 2023 Framework for Health Emergency Prevention, Preparedness, Response, and Resilience (HEPR) with a focus on five “core health emergency components”:
- Collaborative surveillance
- Strong national integrated disease, threat, and vulnerability surveillance,
- Effective diagnostics and laboratory capacity for pathogen and genomic surveillance
- Collaborative approaches for event detection, risk assessment, and response monitoring
- Community protection
- Community engagement, risk communication, and infodemic management
- Population and environmental public health interventions
- Multisectoral action for social and economic protection
- Access to countermeasures
- Fast tracked research and development
- Scalable manufacturing platforms
- Coordinated supply chains and emergency
- Emergency coordination
- Strengthened workforce capacity for health emergencies
- Strengthening health emergency preparedness, readiness, and resilience
- Health emergency alert and response coordination
- Safe and scalable care
- Scalable clinical care during emergencies
- Protection of health workers and patients
- Maintenance of essential health services
How do you think the SPRP can be effectively translated into specific contexts and implemented sustainably?
For insights into vaccination efforts for diseases that are being exacerbated by the effects of climate change, get your tickets to the Congress in Barcelona this month, or subscribe to our weekly newsletters here.