An article in In Vivo in September 2022 explored the development and therapeutic potential of oncolytic viruses. Crediting a “relatively safe mode of action” and possibility of enhancing existing treatments, the article stated that 1/3 or cancer vaccines in development are now oncolytic viruses. Cancer vaccines continue to gain momentum as “immuno-oncology has validated the immune system’s essential role in maintaining healthy cell division”. Thus, researchers have become interested in designing vaccines against cancerous cells as well as infectious diseases.
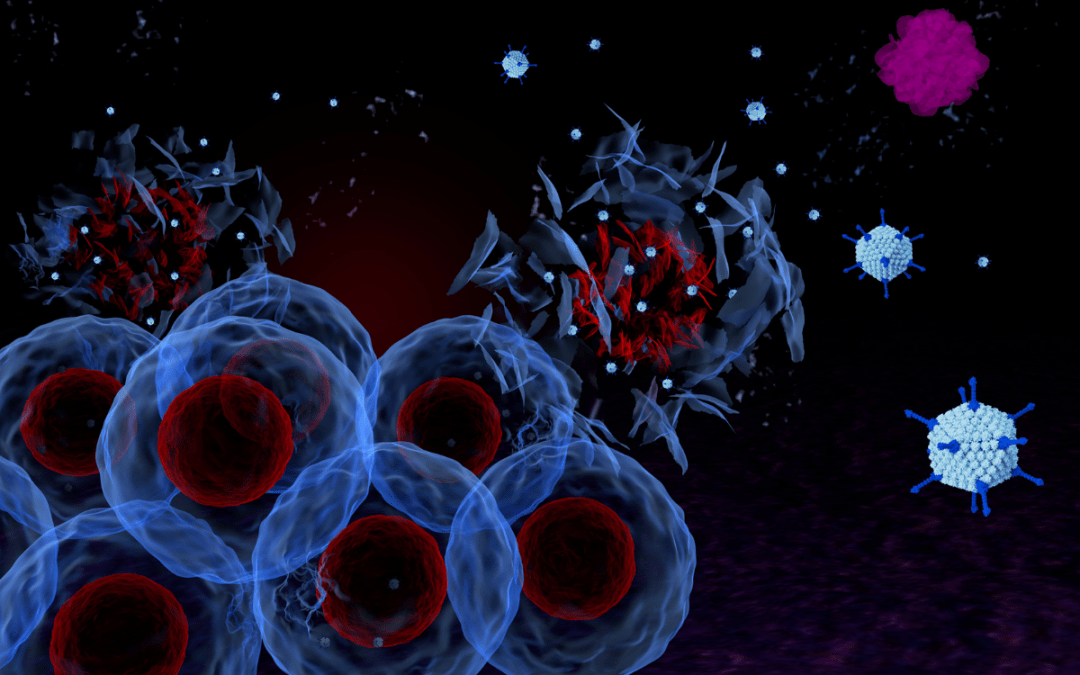
In a previous post we explored how oncolytic viruses (OVs) have the “potential to revolutionise standard cancer treatment”. OVs can “selectively infect cancerous cells, with an additional genetic modification step”. This causes oncolysis and releases intracellular antigens. These antigens “can stimulate an innate immune response that eliminates” further cancerous cells. OVs are “highly targeted”, so have a “limited effect on healthy cells”. The result is that, although they sometime prompt the immune system to turn on healthy cells, they lead to “minimal toxicities”.
The article in In Vivo states that there are “currently 162 OV therapies in active development”. Although the majority are not yet at clinical trial stage, 4 have “successfully navigated through clinical development” to receive regulatory approval.
The approved products
Of the 4 that have gone to market, Imylgic (talimogene laherparepvec) is “the most notable as the first genetically modified OV”. Approved in 2015 by the FDA and the EMA, it is an attenuated herpes simplex virus type-1 vaccine.
Further products include Rigvir, approved in 2004 in Eastern Europe for the treatment of melanoma. Oncorine received approval in China “in conjunction with chemotherapy” against nasopharyngeal cancer. Finally, in 2021 Delytact (teserpaturev) was conditionally approved in Japan for the treatment of malignant glioma.
At present, OV therapies “are not currently approved for use in combination with other therapies”, but this possibility is being explored in clinical trials.
“Combining OVs with other immunotherapies is a sensible approach to achieve additive or synergistic anti-tumour responses and to overcome treatment resistance”.
Furthermore, the “nature of the treatment algorithm” promotes this combination approach as the “most practical way to evaluate an investigational drug in clinical trials”.
What is next for OV therapies?
OV therapies are “the ideal therapy type for cancer” because they are so precise, “preserving healthy cells” whilst targeting tumour cells. However, compared to other types of immunotherapy they “perform poorly”. The article questions whether this is down to “lack of investment” or an “inherently weaker clinical profile”.
As we encountered in IDT Biologika’s white paper on OVs, there are several “developmental drawbacks” that must be overcome in order to accelerate the pipeline process. As this article in In Vivo highlights, realising the potential of OV therapies will require developmental optimisation.
“The future success for OVs will depend upon finding the most appropriate patient populations and combination strategies where clinical benefit will be greatest.”
To learn more about therapeutic cancer vaccines come to the World Vaccine Congress in Europe, October 2022. Get your tickets at this link.